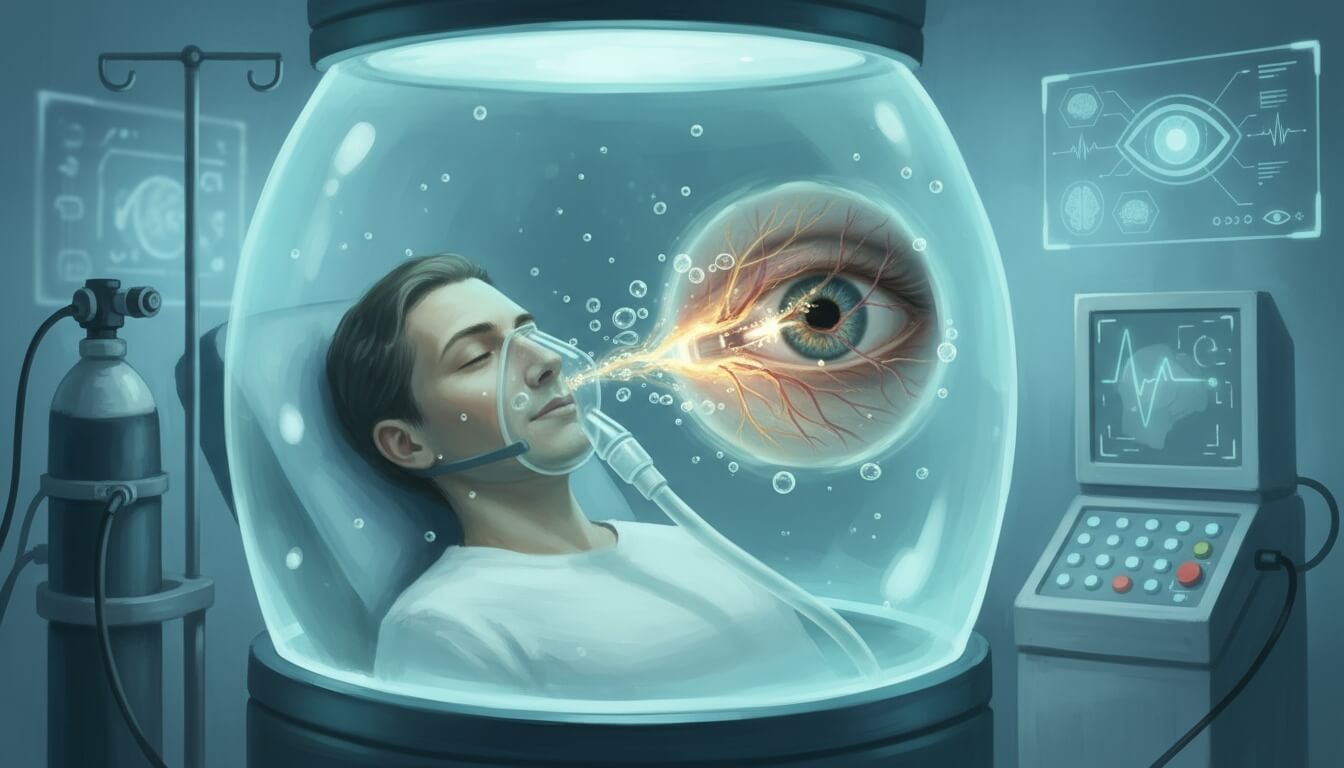
- Patients receiving hyperbaric oxygen therapy (HBOT) showed significantly better visual recovery compared to standard treatment, with 76.5% achieving at least three lines of vision improvement versus 40.6% in the control group.
- The study protocol involved five daily HBOT sessions starting at 2.0 atmospheres absolute (ATA) for 180 minutes, then 2.4 ATA for 90 minutes, regardless of visual changes during treatment.
- Treatment remained effective even when initiated up to 24 hours after symptom onset, challenging previous assumptions about the narrow therapeutic window for central retinal artery occlusion (CRAO).
- Optical coherence tomography (OCT) measurements revealed less retinal thinning in HBOT patients at one month, suggesting the therapy helps preserve retinal structure beyond just functional improvements.
- Two of 17 patients (11.8%) experienced adverse events, including headache with nausea and one seizure case, though both recovered fully without long-term complications.
Researchers at Siriraj Hospital, Mahidol University in Bangkok conducted a retrospective study examining 49 patients diagnosed with CRAO between October 2003 and March 2022. The study, published in Clinical Ophthalmology, compared outcomes between 17 patients who received HBOT and 32 who received standard care alone.
CRAO represents a rare but devastating ophthalmic emergency, affecting approximately one in 100,000 adults annually according to research published in the American Journal of Ophthalmology. The condition shares similarities with stroke, causing sudden vision loss that typically deteriorates to 20/400 or worse in most cases.
Lead author Dr. Supathida Jiamsawad and colleagues established strict inclusion criteria. All patients presented within 24 hours of symptom onset. The team excluded patients who received recombinant tissue plasminogen activator (rt-PA) or experienced treatment-related complications.
Both groups showed comparable baseline characteristics. Initial visual acuity measured 2.3 logarithm of the minimum angle of resolution (logMAR) in both cohorts. Mean symptom onset time was 11.6 hours for HBOT patients and 12.0 hours for controls.
Treatment Protocol and Rationale
The Siriraj protocol differs from previous HBOT approaches in several key aspects. Patients received treatment once every 24 hours for five consecutive days, regardless of visual improvement during therapy.
The first session delivered 100% oxygen at 2.0 ATA for 180 minutes. This included a 15-minute descent period, a five-minute air break midway through treatment, and a 15-minute ascent. Subsequent sessions increased pressure to 2.4 ATA but shortened duration to 90 minutes, maintaining the five-minute air break.
Dr. Jiamsawad explained the rationale in the study. “The lower initial session at 2 ATA mitigates the risk of oxygen toxicity, while compensating for oxygen supply by the longer duration at 180 minutes.”
The 24-hour intervals between sessions aim to trigger what researchers call the hyperoxic-hypoxic paradox. During rest periods, lower oxygen levels stimulate hypoxia-inducible factor (HIF), a transcription factor regulating over 100 genes necessary for cellular survival under oxygen-deprived conditions. This process improves cells’ ability to produce energy independently of oxygen while inducing vascular endothelial growth factor (VEGF) to promote blood vessel formation.
Visual Outcomes and Statistical Analysis
At discharge, 76.5% of HBOT patients achieved visual improvement of at least 0.3 logMAR (three lines on an eye chart) compared to 40.6% in the control group (p = 0.02). Mean visual acuity improved from 2.3 to 1.4 logMAR in the HBOT group, while controls showed modest change from 2.3 to 2.0 logMAR.
The HBOT advantage persisted at follow-up examinations. At one week, mean visual acuity measured 1.5 logMAR for HBOT patients versus 2.1 logMAR for controls. At one month, these values remained 1.4 logMAR and 1.9 logMAR respectively.
Generalized estimation equation (GEE) analysis identified HBOT as a statistically significant predictor of visual outcome (p < 0.01). The treatment showed a coefficient of -0.59 (95% confidence interval: -0.94 to -0.25), meaning HBOT reduced final logMAR by 0.59 units.
Anterior chamber paracentesis also emerged as a significant predictor, with a coefficient of -0.42 (95% CI: -0.70 to -0.15, p < 0.01). However, 76.5% of HBOT patients also received paracentesis, making it difficult to isolate each intervention’s specific contribution.
Structural Preservation Evidence
OCT measurements provided objective evidence of HBOT’s protective effects. Researchers measured inner retinal thickness manually at four quadrants (nasal, temporal, superior, inferior) located 750 micrometers from the fovea.
At initial presentation, mean inner retinal thickness measured 206.8 micrometers in the HBOT group and 192.6 micrometers in controls (p = 0.646). At one month follow-up, HBOT patients maintained significantly greater thickness at 136.3 micrometers compared to 104.3 micrometers in controls (p = 0.049).
The findings suggest HBOT helps preserve retinal structure by mitigating ischemic damage. According to research in Experimental Eye Research, the inner retina relies predominantly on the central retinal artery for oxygen. When this artery becomes blocked, HBOT increases dissolved oxygen in plasma, enabling oxygen to diffuse from the choroidal circulation into ischemic central retina.
This oxygen delivery supports critical retinal layers including ganglion cells, the inner plexiform layer, and the inner nuclear layer. Although HBOT does not restore blood flow through the occluded artery, elevated plasma oxygen allows oxygen to bypass the blockage through diffusion from adjacent capillaries and non-occluded vessels.
Comparison with International Studies
The Thai results align with findings from other countries despite variations in baseline characteristics and treatment timing. Research from Israel by Hadanny and colleagues reported baseline visual acuity of 2.1 logMAR improving to 1.6 logMAR at discharge. German researchers Menzel-Severing and team found improvement from 1.8 logMAR to 1.5 logMAR.
Treatment timing differed substantially between studies. The Israeli cohort began HBOT at mean 7.8 hours after symptom onset, while German patients started at 5.3 hours. Thai patients had significantly longer delays at 11.6 hours, yet achieved similar visual improvements.
Dr. Jiamsawad noted the implications. “Despite this delay, the similar VA improvements suggest that HBOT may still be effective even in patients who present later, reinforcing its potential as a treatment option for CRAO.”
The finding challenges earlier assumptions based on primate experiments by Hayreh and Jonas, which suggested irreversible damage occurs after four hours of complete arterial occlusion. However, human CRAO typically presents as incomplete or temporary occlusion with varying degrees of reperfusion, differing from the experimental model’s direct clamping approach.
Safety Profile and Adverse Events
Two of 17 HBOT patients (11.8%) experienced adverse events. One patient developed headache, nausea, and vomiting before completing the treatment series. Another patient experienced a generalized tonic-clonic seizure lasting one minute during the first session.
Comprehensive evaluation of the seizure patient revealed hypocalcemia as the only notable risk factor. Researchers considered oxygen toxicity the most likely cause. After discussion of risks and benefits, the patient discontinued HBOT and received a short course of antiepileptic medication, which was tapered before discharge.
Both patients recovered fully without requiring further intervention or experiencing long-term complications. No recurrence of symptoms occurred during follow-up. Notably, no patients experienced barotrauma, a common HBOT complication reported in 9% to 27% of cases in various studies.
The relatively low adverse event rate contrasts with risks associated with alternative treatments. Intravenous thrombolysis with rt-PA carries risks of intracerebral and systemic hemorrhage, particularly when administered beyond the 4.5-hour therapeutic window according to American Heart Association guidelines.
Clinical Implications and Treatment Window
The study’s most significant finding may be the extended therapeutic window. Previous recommendations suggested initiating HBOT within 12 hours of CRAO diagnosis, or as early as six to eight hours according to research in the European Journal of Ophthalmology.
GEE analysis revealed that symptom onset time was not a significant predictor of visual outcome (p = 0.41) in patients presenting within 24 hours. This finding aligns with research by Rozenberg and colleagues, which also found no correlation between timing of first HBOT session and final visual outcome in patients presenting within 24 hours.
The extended window provides opportunities for patients who cannot access immediate treatment. Given the time required for hyperbaric chamber preparation, team mobilization, patient evaluation, and standard interventions like ocular massage and paracentesis, the 24-hour window offers more realistic treatment access.
However, the study acknowledges limitations. Despite improvements, mean visual acuity at discharge remained 1.4 logMAR (approximately 6/150 Snellen equivalent) in the HBOT group versus 2.0 logMAR (approximately counting fingers) in controls. Both values fall below the 6/60 threshold defining legal blindness in many countries.
The proportion of patients achieving visual acuity of at least 6/60 remained relatively low in both groups (29.41% HBOT versus 15.6% controls, p = 0.25). This lack of statistical significance suggests that while HBOT produces measurable visual improvement, its impact on achieving functional vision thresholds remains inconclusive.
Study Limitations and Future Directions
The researchers identified several constraints affecting their conclusions. The small sample size of 49 patients limits statistical power. The retrospective design prevented standardized administration of adjunctive treatments between groups.
Follow-up data posed challenges. As a tertiary facility, Siriraj Hospital often refers patients back to initial hospitals for long-term care after acute treatment. This resulted in missing information, particularly one-month visual acuity data. Only 13 of 17 HBOT patients (76.5%) and 27 of 32 controls (84.4%) attended one-month appointments.
OCT analysis faced methodological limitations. Manual measurement of inner retinal thickness, even when divided into quadrants, introduces potential inter-observer variability and measurement bias. The exclusion of poor-quality OCT images relied on subjective determination without predefined quantitative thresholds.
Diagnostic criteria also varied. CRAO diagnosis relied primarily on clinical manifestations supplemented by OCT or fundus fluorescein angiography (FFA) in some cases, but without fully standardized, objective imaging-based criteria used in certain clinical trials.
The study could not isolate HBOT’s specific contribution due to concurrent standard treatments. Most patients received multiple interventions including anti-glaucoma medications, paracentesis, and oxygen therapy. The limited number of patients receiving only HBOT prevented meaningful subgroup analysis.
Dr. Jiamsawad and colleagues emphasize the need for prospective validation. “A study design with more standardized diagnostic protocols, objective image quality criteria, and better control of standard of care represents an important avenue for future research.”
Mechanism of Action and Physiological Basis
HBOT’s therapeutic effect operates through multiple physiological mechanisms. Under normal conditions, 99% of hemoglobin carries oxygen while dissolved free oxygen in plasma remains relatively small. HBOT significantly elevates the dissolved fraction, supplying ischemic areas independently of saturated hemoglobin.
Beyond vascular delivery, aquaporin-1 (AQP-1) water channels serve as alternative oxygen transporters between cells according to research in the Journal of Biological Chemistry. This provides additional pathways for oxygen delivery to hypoxic retinal tissue.
The outer retina, primarily supplied by choroidal circulation, also benefits from increased oxygenation. Photoreceptors with high metabolic demands receive enhanced oxygen delivery from the choroid. By maintaining retinal pigment epithelium and outer retinal layer function, HBOT helps preserve overall retinal integrity, preventing secondary degeneration from inner retinal ischemia.
Some researchers have raised concerns about retinal artery vasoconstriction as a consequence of hyperoxia. However, studies in JAMA suggest vasoconstriction typically occurs only in adequately perfused cells, making it less likely during CRAO’s acute phase when cells face severe oxygen deprivation.
Resource Requirements and Implementation
The fixed five-day protocol offers practical advantages for healthcare facilities. Unlike protocols continuing HBOT until visual improvement plateaus, the standardized approach reduces need for repeated visual acuity evaluations during non-office hours when medical staff are limited.
Predictable scheduling enhances HBOT chamber management, particularly when sharing facilities with other departments. The consistent five-day endpoint ensures treatment cost predictability for patients and healthcare systems.
However, HBOT remains resource-intensive. Treatment requires specialized hyperbaric chambers, trained personnel, and significant time commitment from patients and staff. These requirements limit availability primarily to tertiary care centers.
The study’s setting at Siriraj Hospital, a major academic medical center in Bangkok, may not represent typical resource availability. Smaller facilities or those in rural areas may lack hyperbaric oxygen capabilities, limiting treatment access for many CRAO patients.
Conclusion and Clinical Recommendations
The Siriraj protocol demonstrates that HBOT can improve visual outcomes in CRAO patients presenting within 24 hours of symptom onset. The treatment shows benefits beyond the previously assumed narrow therapeutic window, offering hope for patients unable to access immediate intervention.
The fixed protocol of five daily sessions, starting at 2.0 ATA for 180 minutes then continuing at 2.4 ATA for 90 minutes, provides a practical framework balancing efficacy with safety. The 24-hour intervals between sessions leverage physiological responses to intermittent hypoxia, potentially enhancing long-term cellular survival.
However, the researchers emphasize caution in clinical adoption. “While constrained by the small sample size and short-term outcome data, these results showed the benefits of this unique HBOT protocol in CRAO presenting within the critical 24-hour window. Nevertheless, further prospective validation is necessary before widespread clinical adoption.”
For clinicians managing CRAO patients, HBOT represents a potential option particularly for those presenting outside conventional thrombolysis windows or with contraindications to rt-PA. The therapy may be most valuable when combined with standard interventions like paracentesis, though isolating each treatment’s specific contribution requires further study.
Citations
- Thoongsuwan S, Sirichayaporn T, Rodanant N, et al. Visual Outcomes Following Hyperbaric Oxygen Therapy in Acute Central Retinal Artery Occlusion Patients. Clinical Ophthalmology. 2025. DOI: https://doi.org/10.2147/OPTH.S510772
- Leavitt JA, Larson TA, Hodge DO, Gullerud RE. The incidence of central retinal artery occlusion in Olmsted County, Minnesota. American Journal of Ophthalmology. 2011;152(5):820-823. DOI: https://doi.org/10.1016/j.ajo.2011.05.005
- Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. American Journal of Ophthalmology. 2005;140(3):376-391. DOI: https://doi.org/10.1016/j.ajo.2005.03.038
- Mac Grory B, Schrag M, Biousse V, et al. Management of central retinal artery occlusion: a scientific statement from the American Heart Association. Stroke. 2021;52(6):e282-e294. DOI: https://doi.org/10.1161/STR.0000000000000366
- Hayreh SS, Zimmerman MB, Kimura A, Sanon A. Central retinal artery occlusion. Retinal survival time. Experimental Eye Research. 2004;78:723-736. DOI: https://doi.org/10.1016/S0014-4835(03)00214-8
- Hadanny A, Maliar A, Fishlev G, et al. Reversibility of retinal ischemia due to central retinal artery occlusion by hyperbaric oxygen. Clinical Ophthalmology. 2017;11:115-125. DOI: https://doi.org/10.2147/OPTH.S121307
- Menzel-Severing J, Siekmann U, Weinberger A, Roessler G, Walter P, Mazinani B. Early hyperbaric oxygen treatment for nonarteritic central retinal artery obstruction. American Journal of Ophthalmology. 2012;153(3):454-459. DOI: https://doi.org/10.1016/j.ajo.2011.08.009
- Rozenberg A, Peled A, Hadad A, et al. Hyperbaric oxygen treatment for non-arteritic central retinal artery occlusion retrospective comparative analysis from two tertiary medical centres. Eye. 2022;36(6):1261-1265. DOI: https://doi.org/10.1038/s41433-021-01617-8
- Hayreh SS, Jonas JB. Optic disk and retinal nerve fiber layer damage after transient central retinal artery occlusion: an experimental study in rhesus monkeys. American Journal of Ophthalmology. 2000;129(6):786-795. DOI: https://doi.org/10.1016/S0002-9394(00)00384-6
- Kim YS, Nam MS, Park EJ, et al. The effect of adjunctive hyperbaric oxygen therapy in patients with central retinal artery occlusion. Undersea and Hyperbaric Medicine. 2020;47(1):57-64. DOI: https://doi.org/10.22462/01.03.2020.7
- Beiran I, Goldenberg I, Adir Y, Tamir A, Shupak A, Miller B. Early hyperbaric oxygen therapy for retinal artery occlusion. European Journal of Ophthalmology. 2001;11(4):345-350. DOI: https://doi.org/10.1177/112067210101100405
- Echevarria M, Munoz-Cabello AM, Sanchez-Silva R, Toledo-Aral JJ, Lopez-Barneo J. Development of cytosolic hypoxia and hypoxia-inducible factor stabilization are facilitated by aquaporin-1 expression. Journal of Biological Chemistry. 2007;282(41):30207-30215. DOI: https://doi.org/10.1074/jbc.M702639200
- Saltzman HA, Hart L, Sieker HO, Duffy EJ. Retinal vascular response to hyperbaric oxygenation. JAMA. 1965;191(4):290-292. DOI: https://doi.org/10.1001/jama.1965.03080040032007
The research adds to growing evidence supporting HBOT for CRAO while highlighting the need for larger, prospective trials with standardized protocols and longer follow-up periods to establish definitive treatment guidelines.