Depression affects one in three people at some point in their lives [1]. Despite decades of pharmaceutical advances, traditional antidepressants fail to help roughly 30% of patients. Psychotherapy shows promise but requires months or years to produce results. What happens when pills don’t work and talk therapy stalls?
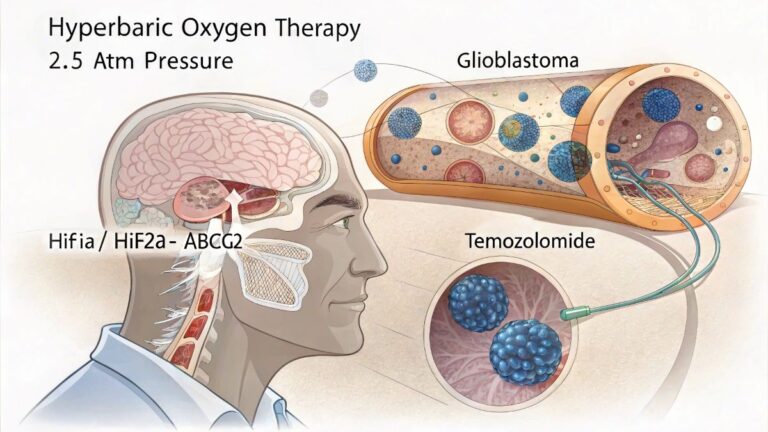
Enter hyperbaric oxygen therapy (HBOT) – a treatment originally designed for decompression sickness that’s now showing potential for rewiring depressed brains. Patients breathe pure oxygen in pressurized chambers, and emerging research suggests this simple intervention might spark neurological changes that lift persistent sadness.
The science isn’t settled, but early findings paint an intriguing picture. Military veterans with traumatic brain injuries report dramatic mood improvements after HBOT sessions. Stroke survivors see their depression scores plummet. Post-injury patients who combine oxygen therapy with traditional treatments recover faster than those using medications alone.
What is Hyperbaric Oxygen Therapy (HBOT)
HBOT involves breathing 100% oxygen while sitting in a pressurized chamber. The atmospheric pressure increases to 1.5-3 times normal sea level pressure. Sessions typically last 60-90 minutes, and patients often need 20-40 treatments over several weeks [2].
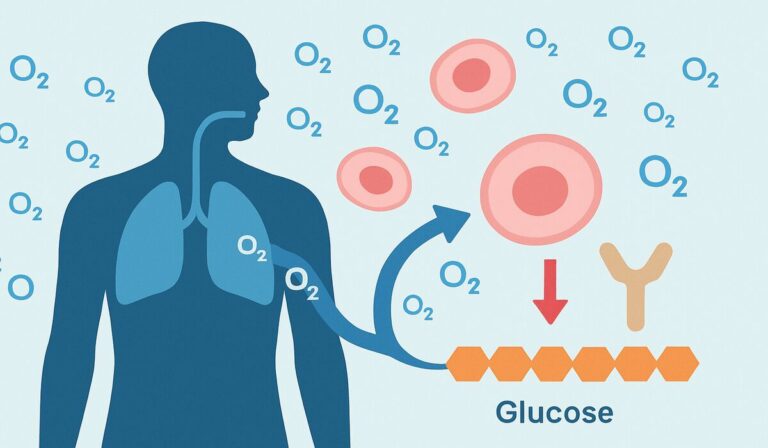
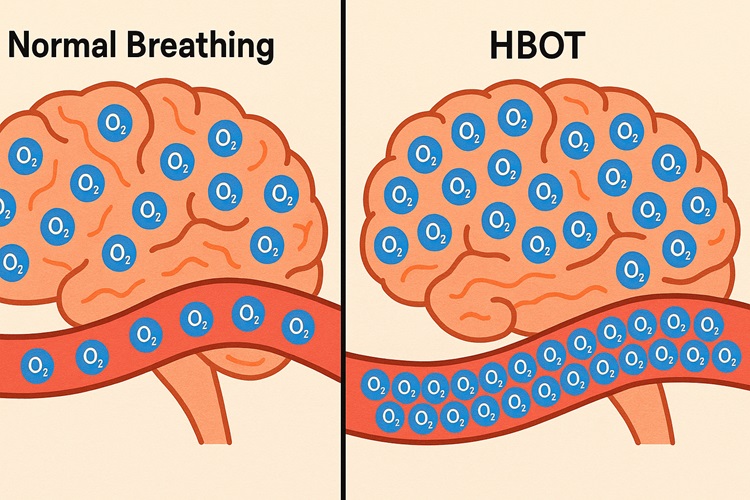
The process sounds simple, but the physiological effects run deep. Under pressure, oxygen dissolves into blood plasma at much higher concentrations than normal breathing allows. This oxygen-rich blood reaches brain tissue that standard circulation might miss.
Think of it like this: normal breathing = delivering oxygen via standard mail. HBOT = express delivery to every corner of your brain.
How HBOT Affects the Brain to Combat Depression
Boosting Brain Oxygenation to Enhance Cellular Function
Depressed brains often show reduced metabolism in key regions like the prefrontal cortex and hippocampus. HBOT floods these areas with oxygen, allowing neurons to produce more energy and function normally [3]. Brain scans reveal increased activity in previously underperforming regions after treatment.
Mitigating Neuroinflammation: A Key Contributor to Depression
Chronic inflammation disrupts brain chemistry and contributes to persistent low mood [4]. HBOT reduces inflammatory markers and calms overactive immune responses in neural tissue. This anti-inflammatory effect may explain why some patients see mood improvements lasting months after treatment ends [5].
Fostering Neurogenesis: The Growth of New Brain Cells
Depression shrinks the hippocampus – the brain region handling memory and emotion. HBOT stimulates the production of brain-derived neurotrophic factor (BDNF) and activates neurogenesis pathways [6]. New neurons begin sprouting in areas damaged by chronic stress and depression.
Optimizing Cerebral Blood Flow for Improved Brain Health
HBOT promotes angiogenesis = formation of new blood vessels. Better vascularization means improved nutrient delivery and waste removal from brain tissue [7]. Enhanced blood flow also supports the growth and survival of newly generated neurons.
The Scientific Evidence on HBOT for Depression
2017 Study on Spinal Cord Injury, Depression, and Anxiety
Researchers compared HBOT to psychotherapy in 60 patients with spinal cord injuries and co-occurring depression [8]. After eight weeks, both groups showed significant symptom reduction, but the HBOT group improved faster. Depression scores dropped by an average of 12 points on standardized scales. Anxiety symptoms decreased by 35% compared to baseline measurements.
2015 Study on Post-Stroke Depression
This randomized controlled trial examined 90 stroke survivors with major depression [9]. Participants received either antidepressants alone, HBOT alone, or combined treatment. The combination group showed the most dramatic improvement – 65% achieved remission versus 40% in the medication-only group. HBOT appeared to amplify antidepressant effectiveness.
Systematic Review on HBOT for PTSD and TBI
Multiple studies tracked military personnel with traumatic brain injuries and PTSD [10][11]. Veterans receiving HBOT reported 40-50% reductions in depression scores. Suicidal ideation decreased significantly, and quality of life measures improved across the board. (Ed. note: These studies often included small sample sizes, so results should be interpreted cautiously.)
Systematic Review on New Biological Treatments
A comprehensive analysis of emerging depression therapies concluded that HBOT shows “promising but preliminary” evidence [12]. While research remains in early stages, current data suggests oxygen therapy may enhance traditional antidepressant responses and provide standalone benefits for certain patient populations.
Study on HBOT for Depression after Cerebral Hemorrhage
Patients recovering from brain hemorrhages who received HBOT plus standard care showed 60% greater improvement in depression symptoms compared to controls [13]. Neurological function also improved more rapidly in the HBOT group, suggesting broad brain health benefits beyond mood enhancement.
When you step back and look at the complete picture, several patterns emerge. First, HBOT consistently demonstrates depression-fighting effects across diverse patient populations = from spinal cord injury survivors to stroke patients to military veterans.
Second, the treatment appears most effective when combined with other interventions rather than used in isolation. Third, brain imaging studies repeatedly show that clinical improvements correlate with measurable changes in brain structure and function.
The evidence isn’t bulletproof yet, but it’s building momentum. We’re seeing consistent results from different research groups using varying protocols, which strengthens confidence in HBOT’s therapeutic potential.
What to Expect from HBOT Treatment
Your first appointment involves comprehensive medical screening. Doctors review your psychiatric history, current medications, and physical health status. They’ll assess whether you’re a good candidate and explain potential risks. Some providers require psychological evaluations before starting treatment.
A Walkthrough of a Typical HBOT Session
You enter a clear chamber that looks like a transparent tube or room. Technicians gradually increase the pressure over 10-15 minutes – your ears might pop like during airplane descent. You breathe normally through a mask delivering pure oxygen. Many patients read, listen to music, or nap during sessions.
Pressure decreases slowly at session’s end to prevent decompression sickness. The whole process takes 90-120 minutes including setup and decompression time.
Standard Treatment Protocols for Depression
Most depression protocols involve 20-40 sessions over 4-8 weeks. Sessions occur daily or every other day. Pressure typically ranges from 1.5-2.5 atmospheres absolute (ATA). Treatment duration may extend based on individual response and symptom severity.
Some patients notice mood improvements within the first week. Others require several weeks to see significant changes. “Am I expecting too much too soon?” This question comes up frequently – patience often determines treatment success.
Is HBOT the Right Choice for You?
HBOT works best for patients with treatment-resistant depression, especially those with brain injuries or inflammatory conditions [14]. Candidates should be medically stable and able to handle pressure changes. People with certain lung conditions, recent ear surgeries, or untreated pneumothorax cannot safely undergo treatment.
Common Side Effects
Common side effects include ear pressure, temporary vision changes, and mild claustrophobia. Serious complications are rare but can include oxygen toxicity or pneumothorax (collapsed lung). Facilities must have emergency protocols and trained medical staff on-site.
Who Should Not Undergo HBOT?
Absolute contraindications include untreated pneumothorax, certain medications, and severe lung diseases. Pregnancy requires special consideration. Patients with pacemakers or other implanted devices need clearance from their cardiologist.
HBOT vs. Pharmacotherapy
Antidepressants work by altering neurotransmitter levels, while HBOT targets oxygen delivery and neuroinflammation. Pills take 6-8 weeks to show effects; HBOT may produce faster results. Side effects differ dramatically – sexual dysfunction and weight gain are common with medications, while HBOT’s main risks involve pressure-related complications.
Cost presents a major difference. Monthly antidepressant prescriptions run $20-200, while HBOT courses can cost thousands of dollars.
Combining HBOT with Psychotherapy
Research suggests HBOT and therapy complement each other well [15]. Improved brain oxygenation may enhance cognitive flexibility needed for therapeutic breakthroughs. Many providers recommend continuing counseling throughout HBOT treatment.
Transcranial magnetic stimulation (TMS) and ketamine therapy
Transcranial magnetic stimulation (TMS) and ketamine therapy target different brain mechanisms than HBOT. TMS uses magnetic fields to stimulate specific brain regions. Ketamine rapidly alters glutamate signaling. Some clinics offer combination protocols, though research on these approaches remains limited.
Insurance, Costs, and Provider Selection
A Detailed Breakdown of HBOT Costs
Individual HBOT sessions cost $200-500 at medical facilities. Complete treatment courses range from $4,000-20,000 depending on session number and facility location. Hospital-based programs typically charge more than standalone hyperbaric centers.
What Is and Isn’t Covered for HBOT Depression Treatment
Most insurance plans don’t cover HBOT for depression since it’s considered experimental. Medicare and private insurers approve HBOT for specific conditions like diabetic wounds and carbon monoxide poisoning, but mental health applications remain off-label. Some patients use health savings accounts or payment plans to manage costs.
Where to Find Credible and Experienced HBOT Providers?
Look for facilities accredited by the Undersea and Hyperbaric Medical Society (UHMS). Staff should include board-certified hyperbaric physicians and trained technicians. Ask about safety protocols, emergency procedures, and experience treating depression specifically.
Check online reviews but focus on safety records rather than testimonials. State health departments maintain facility inspection reports you can review.
Considering Buying an HBOT Chamber for Home Use
Portable chambers cost $15,000-30,000 for basic models. While convenient, home units typically operate at lower pressures than clinical chambers. Safety concerns include lack of medical supervision and emergency response capabilities.
Most depression research used hospital-grade equipment, so home chambers may not provide equivalent benefits.
Frequently Asked Questions
“Won’t this just be another expensive disappointment?”
This concern reflects reasonable caution given the mixed track record of depression treatments. HBOT isn’t a magic bullet, but emerging research suggests it offers genuine promise for specific patient populations.
Conclusion
HBOT addresses depression through multiple biological pathways – increasing brain oxygenation, reducing inflammation, promoting neurogenesis, and enhancing blood flow. Research shows promising results, particularly for treatment-resistant cases and patients with brain injuries.
Safety risks are manageable with proper medical supervision, but costs remain high and insurance coverage limited. The treatment works best as part of comprehensive care rather than standalone therapy.
Consider HBOT if traditional treatments have failed and you can afford the investment. Discuss the option with your psychiatrist or primary care physician. Research local facilities and verify their credentials. Remember that newer doesn’t always mean better – HBOT shows promise but isn’t proven superior to established treatments for most patients.
The field continues evolving rapidly. What seems experimental today might become standard care tomorrow. Stay informed about emerging research while making decisions based on current evidence and your specific circumstances.
References
[1] NCBI Bookshelf – “Hyperbaric Oxygen Therapy for Adults with Mental Illness: A Review of the Clinical Effectiveness” – August 27, 2014
[2] Frontiers in Neurology – “Hyperbaric oxygen therapy as a neuromodulatory technique: a review of the recent evidence” – August 23, 2024
[3] PMC – “Hyperbaric oxygen therapy as a neuromodulatory technique: a review of the recent evidence” – 2024
[4] Scientific Reports – “Normobaric oxygen treatment for mild-to-moderate depression: a randomized, double-blind, proof-of-concept trial” – September 23, 2021
[5] PMC – “Whole Body Cryotherapy and Hyperbaric Oxygen Treatment: New Biological Treatment of Depression? A Systematic Review” – 2021
[6] PMC – “Effects of hyperbaric oxygen therapy on depression and anxiety in the patients with incomplete spinal cord injury (a STROBE-compliant article)” – 2017
[7] Neuropsychology Review – “Impact of Hyperbaric Oxygen Therapy on Cognitive Functions: a Systematic Review” – April 13, 2021
[8] PubMed – “Effects of hyperbaric oxygen therapy on depression and anxiety in the patients with incomplete spinal cord injury (a STROBE-compliant article)” – 2017
[9] PubMed – “Hyperbaric oxygen therapy for post-stroke depression: A systematic review and meta-analysis” – 2020
[10] PMC – “Hyperbaric Oxygen Treatment—From Mechanisms to Cognitive Improvement” – 2021
[11] Scientific Reports – “Hyperbaric oxygen therapy improves neurocognitive functions and symptoms of post-COVID condition: randomized controlled trial” – July 12, 2022
[12] Journal of Neuroinflammation – “Neuroinflammation, memory, and depression: new approaches to hippocampal neurogenesis” – November 27, 2023
[13] PMC – “Efficacy of hyperbaric oxygen treatment for depression in the convalescent stage following cerebral hemorrhage” – 2013
[14] PubMed – “Hyperbaric Oxygen Therapy for Adults with Mental Illness: A Review of the Clinical Effectiveness” – August 27, 2014
[15] Translational Psychiatry – “Neuroinflammation mechanisms of neuromodulation therapies for anxiety and depression” – January 9, 2023