Hyperbaric Oxygen Therapy (HBOT) might sound like something from a science fiction movie, but it’s actually a well-established medical treatment that’s been helping patients for decades. In its simplest form, HBOT involves breathing pure oxygen in a pressurized environment.
Just imagine yourself sitting in a special room or chamber where the air pressure is increased to two or three times higher than normal atmospheric pressure.
When you’re inside a hyperbaric chamber, your lungs gather much more oxygen than would be possible breathing pure oxygen at normal air pressure. This extra oxygen gets dissolved into your blood plasma, allowing it to reach areas where blood flow is reduced or blocked.
In this comprehensive article, we’re taking an introductory deep dive into the world of Hyperbaric Oxygen Therapy and how it can help people become healthier.
The Science Behind Hyperbaric Oxygen Therapy
How Pressure Affects Oxygen Dissolution
To understand what makes HBOT so effective, we need to explore a principle of physics called Henry’s Law. This law states that the amount of gas dissolved in a liquid is proportional to the pressure of that gas above the liquid. In simpler terms, when you increase the pressure, you can dissolve more gas in a liquid.

In our bodies, this means that under the increased pressure of a hyperbaric chamber, your blood plasma (the liquid portion of your blood) can dissolve significantly more oxygen. At normal pressure, your red blood cells do most of the heavy lifting when it comes to carrying oxygen. But in a hyperbaric environment, your plasma becomes a major oxygen carrier too.
This is very important because red blood cells can only go where blood vessels allow them to travel. In damaged tissues, blood vessels might be blocked or compressed. Oxygen dissolved in plasma, however, can diffuse more easily into these compromised areas, delivering its healing properties directly to cells in need.
Cellular Mechanisms of HBOT
At the cellular level, the effects of HBOT are truly remarkable. When tissues receive this surge of oxygen, several beneficial processes kick into gear:
- Enhanced white blood cell activity improves your body’s ability to fight infections.
- New blood vessel formation (angiogenesis) is stimulated in areas with reduced blood flow. [1]
- Stem cell mobilization from bone marrow increases, promoting tissue repair. [2]
- Production of growth factors and collagen accelerates, helping wounds heal faster.
- Harmful bacteria that cannot survive in high-oxygen environments are killed. [3]
The increased oxygen levels also reduce inflammation and swelling by causing blood vessels to constrict while still delivering more oxygen to tissues – a seemingly paradoxical effect that makes HBOT particularly useful for conditions involving inflammation.
Recent research has shown that HBOT can even influence gene expression, turning on genes involved in growth and repair while turning off those that contribute to inflammation and cell death.
History and Evolution of Hyperbaric Medicine
The history of hyperbaric medicine stretches back much further than many people realize. The concept of using pressurized environments for health benefits dates back to the 1600s when British clergyman Henshaw built the first documented pressurized room called a “domicilium.” He didn’t fully understand the science, but he believed that pressure could help with respiratory diseases. [4]
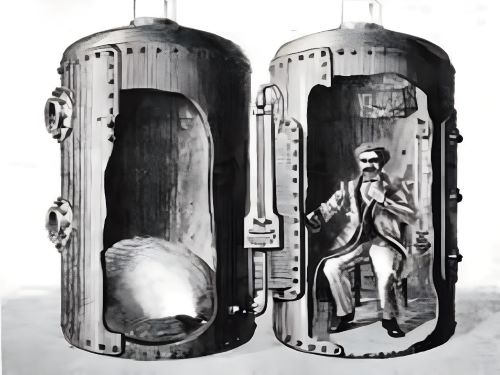
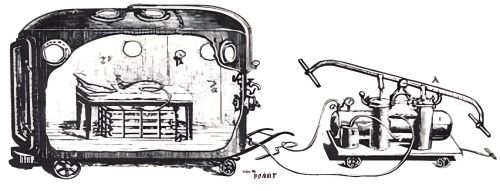
The true medical applications of hyperbaric therapy began to emerge in the 19th century. French surgeon Fontaine built a pressurized mobile operating room in 1879, finding that patients experienced less pain and bleeding during surgery. [4]
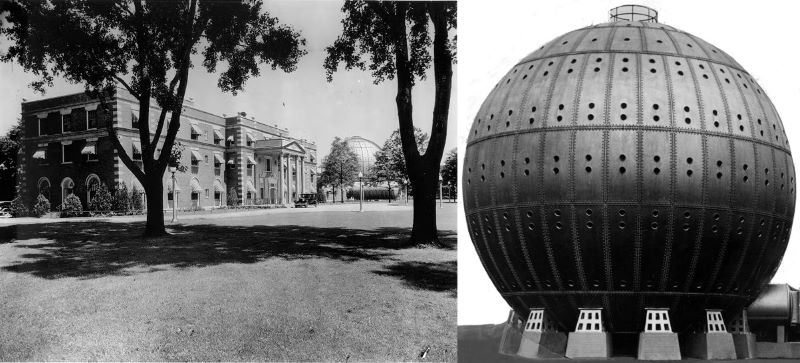
The field took a significant leap forward in the early 20th century when Dr. Orville Cunningham used hyperbaric oxygen to successfully treat someone dying from the flu during the pandemic of 1918. [4]
In his enthusiasm, Cunningham later built a massive hyperbaric chamber called the “Steel Ball Hospital” in Cleveland, Ohio – a structure five stories high that unfortunately became more of a novelty than a medical facility.
The modern era of hyperbaric medicine began in earnest in the 1940s when the military adopted it for treating decompression sickness in divers. By the 1960s, the therapeutic benefits for other conditions started becoming apparent. [5]
The Undersea and Hyperbaric Medical Society (UHMS) was established in 1967 to further research and establish protocols, helping transform HBOT from an experimental treatment to a mainstream medical therapy. [6]
Today, there are over 1,200 hyperbaric facilities in the United States alone, with ongoing research constantly expanding our understanding of how and when this therapy can be most effective.
Types of Hyperbaric Chambers
Monoplace Chambers

The most common type of hyperbaric chamber you’ll encounter in hospitals and dedicated treatment centers is the monoplace chamber. These tube-shaped devices are designed for a single person to lie down inside. Made of clear acrylic, they allow you to see outside during treatment, which helps reduce anxiety and claustrophobia.
In a monoplace chamber, you lie on a padded table that slides into the tube. The entire chamber is then pressurized with 100% oxygen, meaning you breathe the oxygen directly without any mask or hood. These chambers typically operate at pressures between 2 and 3 atmospheres absolute (ATA).
The advantages of monoplace chambers include their relatively lower cost, smaller footprint, and simpler operation. However, they do limit the ability for medical staff to directly access you during treatment, though communication systems allow you to speak with the operator at all times.
Multiplace Chambers

For more intensive medical applications, multiplace chambers provide a different approach. These larger chambers can accommodate multiple patients simultaneously, along with medical staff who can provide hands-on care during treatment.
Unlike monoplace chambers, multiplace units are pressurized with air, and patients breathe pure oxygen through masks, hoods, or endotracheal tubes. This approach allows medical staff to work in the chamber without being exposed to high oxygen levels for extended periods, which could pose safety risks.
Multiplace chambers can typically reach higher pressures than monoplace units and are the preferred choice for treating critically ill patients or those requiring direct medical attention during therapy. They’re commonly found in major medical centers and specialized hyperbaric treatment facilities.
Portable Hyperbaric Chambers

A third category has emerged in recent years: portable or mild hyperbaric chambers (mHBOT). These soft-shelled chambers can be used at home and typically provide much lower pressures (around 1.3 ATA) and use filtered ambient air rather than pure oxygen.
It’s important to note that these portable chambers are not FDA-approved for most medical conditions treated by traditional HBOT. They’re primarily cleared for treating altitude sickness and are sometimes used for athletic recovery, though the evidence for these applications is still developing.
While they may provide some mild benefits, portable chambers should not be considered equivalent to medical-grade HBOT for serious conditions. Some users report subjective improvements for various complaints, but the science supporting these uses lags behind the marketing claims often made about these devices.
Medical Conditions Treated with HBOT
FDA-Approved Indications
The Food and Drug Administration (FDA) has approved HBOT for treating a specific list of conditions where strong scientific evidence supports its use. These include:
- Decompression sickness (“the bends”) in divers
- Gas embolism (air bubbles in blood vessels)
- Carbon monoxide poisoning
- Gas gangrene (a life-threatening bacterial infection)
- Crushing injuries and traumatic ischemias (compromised blood flow)
- Radiation injury, such as damage to tissues following cancer treatment
- Compromised skin grafts and flaps
- Chronic non-healing wounds, particularly diabetic foot ulcers
- Severe anemia where blood transfusion isn’t possible
- Intracranial abscess (brain infection)
- Osteomyelitis (bone infection) that hasn’t responded to standard treatment
- Thermal burns
- Sudden hearing loss
For these approved conditions, HBOT is generally covered by insurance and has demonstrated clear benefits in clinical trials and decades of medical practice.
Off-Label Uses Being Researched
Beyond these established applications, researchers are investigating HBOT’s potential for a much wider range of conditions. Some of the most promising areas include:
- Traumatic brain injury and concussion recovery
- Stroke rehabilitation
- Long COVID symptoms
- Autism spectrum disorders
- Lyme disease and other chronic infections
- Fibromyalgia and chronic fatigue syndrome
- Inflammatory bowel diseases
- Post-surgical recovery
- Migraine headaches
- Multiple sclerosis
- Alzheimer’s disease and vascular dementia
The evidence for these applications varies widely, with some showing promising early results in small studies while others remain highly controversial. Patients considering HBOT for off-label uses should approach the treatment with realistic expectations and understand that insurance often won’t cover these applications.
The HBOT Treatment Experience

What to Expect During a Session
If you’re scheduled for hyperbaric oxygen therapy, knowing what to expect can help ease any anxiety. The experience is generally straightforward and non-invasive, though it may feel unusual at first.
Before your session, you’ll need to remove all electronic devices, jewelry, and other items that could pose a fire risk in the oxygen-rich environment. You’ll typically wear a hospital gown or cotton clothing provided by the facility. Your medical team will check your vital signs and may examine your ears and sinuses, as pressure changes can affect these areas.
Once inside the chamber, you’ll lie comfortably on a padded table. In a monoplace chamber, the door will be secured, and you’ll hear the sound of oxygen beginning to flow. As the chamber pressurizes (called “compression”), you’ll feel fullness in your ears similar to what you might experience when landing in an airplane. Swallowing, yawning, or using equalization techniques can help relieve this pressure.
During the treatment, which typically lasts between 90 minutes and two hours, you can rest, sleep, or watch a movie on a screen provided by some facilities. The chamber remains transparent, so you can see the medical staff outside, and communication systems allow you to speak with them if needed.
At the end of the session, the chamber will slowly depressurize (called “decompression”), and you might again feel the need to equalize your ears. After exiting the chamber, staff will check your vital signs again before you leave.
Treatment Protocols and Duration
HBOT treatment isn’t a one-and-done solution. For most conditions, you’ll need multiple sessions to achieve optimal results. The exact protocol varies depending on your condition:
- For acute conditions like carbon monoxide poisoning or decompression sickness, you might need only 1-3 intensive treatments.
- For radiation injuries, a typical course might include 30-40 daily sessions at 2.0-2.4 ATA for 90-120 minutes each.
- For diabetic foot ulcers or other chronic wounds, expect 20-40 sessions, often scheduled 5 days per week.
- For neurological conditions being treated off-label, protocols can range from 40-80 sessions or more.
The pressure levels, session duration, and frequency are all carefully calculated based on your specific condition and response to treatment. Your doctor might adjust the protocol as treatment progresses, especially if you’re experiencing side effects or showing particularly good or poor response.
Full treatment courses can span weeks or months, requiring a significant time commitment. However, most patients can return to normal activities immediately after each session, as there’s typically no recovery time needed.
Potential Benefits of Hyperbaric Oxygen Therapy
The wide range of conditions HBOT can help reflects its fundamental mechanism: enhancing the body’s natural healing processes through oxygen saturation.
Some of the most remarkable benefits include:
- Accelerated wound healing is perhaps the most visible benefit. For people with diabetic foot ulcers or radiation injuries that won’t heal with standard care, HBOT can make the difference between recovery and amputation.
- The anti-inflammatory effects can be life-changing for people suffering from conditions with chronic inflammation. By reducing swelling and promoting normal blood vessel function, HBOT helps tissues return to healthier states.
- HBOT’s ability to kill anaerobic bacteria (those that thrive without oxygen) makes it powerfully effective against certain serious infections. For necrotizing fasciitis (flesh-eating disease) or gas gangrene, it can be part of a life-saving treatment approach.
- The neurological benefits are among the most exciting and actively researched. By improving oxygen delivery to damaged brain tissue and stimulating neurogenesis (the creation of new brain cells), HBOT may help the brain recover from injuries once thought permanent. Recent research published in PLOS ONE suggests HBOT can improve cognitive function even years after the original brain injury occurred.
- Enhanced immune function is another key benefit, with studies showing HBOT can improve the functioning of immune cells and increase their ability to fight infection.
Perhaps most importantly, HBOT often helps when other treatments have failed. For patients facing limited options, it can offer hope and tangible improvements in quality of life.
Risks and Side Effects of HBOT
While HBOT is generally safe when properly administered, it does carry some risks and potential side effects that patients should be aware of:
- Ear and sinus barotrauma is the most common side effect, occurring when patients have difficulty equalizing pressure during compression or decompression. This can range from mild discomfort to serious injury to the eardrum in rare cases. Patients with colds, allergies, or sinus infections may need to postpone treatment.
- Temporary nearsightedness (myopia) affects some patients due to changes in the eye’s lens from oxygen exposure. This typically resolves within weeks after completing treatment.
- Claustrophobia can be an issue, particularly in monoplace chambers. Mild sedatives may be prescribed for affected patients, or they might be better suited for multiplace chambers.
- Oxygen toxicity is rare but possible with extended exposure to high oxygen levels. Symptoms can include dizziness, nausea, muscle twitching, vision changes, and in extreme cases, seizures. This risk is carefully managed by limiting session duration and using appropriate pressure levels.
- Fire risk is a serious consideration due to the oxygen-rich environment. This is why strict protocols exist regarding what can be brought into chambers.
- Decompression sickness can theoretically occur with certain treatment protocols, though this is extremely rare in medical HBOT settings.
- Pulmonary barotrauma (lung damage) is a risk for patients with certain lung conditions like untreated pneumothorax (collapsed lung). This is why thorough medical screening is essential before beginning treatment.
Fortunately, serious complications are rare when proper screening is conducted and protocols are followed. The overall complication rate is estimated at less than 0.01% for serious adverse events, making HBOT safer than many medical procedures.
Cost and Insurance Coverage
The financial aspects of HBOT can be significant and vary widely depending on your condition and location. For FDA-approved indications, many insurance plans, Medicare, and Medicaid will cover treatment, though you may still have copays or deductibles.
Average costs per session range from $250 to $450 for hospital-based treatments, with a full course potentially costing $10,000 or more. Private clinics sometimes offer lower rates, typically $150-$300 per session.
For off-label conditions, insurance coverage is rare, meaning patients must often pay out-of-pocket. Some clinics offer package deals or financing options to make treatment more accessible.
When pursuing insurance coverage, proper documentation is crucial. Your provider will need to clearly demonstrate medical necessity and show that conventional treatments have been tried without success. Some patients find success with appeals if initially denied coverage.
It’s worth noting that the long-term cost analysis may favor HBOT in some cases. For example, the cost of treating a diabetic foot ulcer with HBOT may be high, but it’s typically much lower than the cost of amputation and subsequent rehabilitation.
Finding a Reputable HBOT Provider
If you’re considering HBOT, finding a qualified provider is essential for both safety and efficacy. Here are key factors to consider:
- Look for facilities accredited by the Undersea and Hyperbaric Medical Society (UHMS). This certification ensures the facility meets strict safety and practice standards.
- The medical director and supervising physicians should be board-certified in Undersea and Hyperbaric Medicine or have extensive specialized training in the field.
- For medical conditions, hospital-based programs generally provide the most comprehensive care, with emergency capabilities if needed. Independent clinics may be appropriate for less acute conditions.
- Ask about the specific protocols they use for your condition. These should align with established guidelines from organizations like the UHMS.
- Facilities should be transparent about success rates, potential side effects, and what to expect during treatment. Be wary of any provider making guarantees or claims that sound too good to be true.
- Experienced technicians and support staff are vital for safe operation and monitoring during treatment.
- Consider practical factors like location, scheduling flexibility, and amenities that might make multiple sessions more comfortable.
- A reputable provider will coordinate with your other healthcare providers and should require a physician referral for treatment.
The Undersea and Hyperbaric Medical Society maintains a directory of accredited facilities on their website, providing a good starting point for your search.
HBOT vs. Other Oxygen Therapies
It’s important to distinguish HBOT from other oxygen delivery methods, as they work quite differently:
- Standard oxygen therapy delivers oxygen at normal atmospheric pressure through nasal cannulas or masks. While helpful for many conditions, it cannot achieve the high dissolved oxygen levels in plasma that HBOT provides.
- Topical oxygen therapy applies oxygen directly to wounds but doesn’t create systemic effects throughout the body.
- Exercise with oxygen therapy (EWOT) involves breathing concentrated oxygen during exercise. While it may increase oxygen levels temporarily, it cannot match the pressure-driven dissolution effects of HBOT.
- Ozone therapy uses a different form of oxygen (O₃ instead of O₂) and lacks the substantial clinical evidence supporting HBOT.
The key differentiator is pressure. Only HBOT combines elevated pressure with 100% oxygen to achieve supersaturation of bodily fluids with dissolved oxygen. This fundamental difference explains why HBOT can help in situations where other oxygen therapies might fall short.
However, HBOT isn’t always the best choice. For chronic lung diseases like COPD, standard oxygen therapy is often more appropriate and safer. Each approach has its place in medical care, and they should be viewed as complementary rather than competing therapies.
Conclusion
Hyperbaric Oxygen Therapy represents a fascinating intersection of physics, physiology, and medicine. By harnessing the simple principle that pressure changes how our bodies absorb and use oxygen, HBOT offers unique healing possibilities for conditions ranging from diving emergencies to chronic wounds, from radiation injuries to brain trauma.
While not a miracle cure, HBOT has earned its place in modern medicine through decades of research and clinical experience. For approved indications, it’s a well-established therapy with clear benefits and manageable risks. For emerging applications, it shows tremendous promise, though more research is needed to fully understand its potential and limitations.
If you’re considering HBOT, approach it with informed optimism. Work with qualified medical providers, understand the evidence for your specific condition, and have realistic expectations about outcomes. For many patients, HBOT has provided healing when other approaches failed, but it works best as part of a comprehensive treatment plan rather than a standalone solution.
As research continues and technology improves, HBOT is likely to become an increasingly important tool in medicine’s arsenal. The simple act of breathing oxygen under pressure continues to reveal new possibilities for healing body and brain.




