Your body possesses an extraordinary ability to heal itself – but sometimes it needs a boost. Enter hyperbaric oxygen therapy (HBOT), a medical treatment that harnesses the power of pressurized oxygen to accelerate cellular repair, reduce inflammation, and help your body heal from the inside out.
By breathing 100% oxygen at pressures 1.5 to 3 times normal atmospheric pressure, HBOT super-saturates your blood with healing oxygen, reaching tissues that conventional treatments can’t touch.
Think of HBOT as giving your cells a turbo-charged oxygen supply. While your red blood cells can only carry so much oxygen under normal conditions, the increased pressure during HBOT dissolves dramatically more oxygen directly into your blood plasma – up to 15-20 times the normal amount [1].
This oxygen-rich environment triggers a cascade of healing processes that can transform how your body recovers from injury, fights infection, and even combats the effects of aging.
How HBOT Works at a Cellular Level

Microscopic cellular view showing oxygen molecules penetrating cells.Here’s where physics meets healing magic. Under normal atmospheric pressure, your blood plasma contains about 0.3 mL of dissolved oxygen per 100 mL of blood. But crank up the pressure to 2.5 atmospheres (typical for HBOT), and that number skyrockets to 5-6 mL per 100 mL – a massive increase that follows Henry’s Law of gas dissolution [2].
This isn’t just academic science. At 3 atmospheres pressure, dissolved oxygen alone can meet your body’s resting metabolic needs, completely independent of hemoglobin transport.
Dr. Ite Boerema proved this dramatically in 1959 with his famous “Life Without Blood” experiment, where animals survived on dissolved oxygen alone after complete blood removal [3].
The real magic happens when this oxygen-rich blood reaches compromised tissues. Areas with poor circulation, scar tissue, or infection suddenly get flooded with healing oxygen that can diffuse directly through plasma.
While normal arterial oxygen measures around 100 mmHg, HBOT can elevate it to 1,400-2,000 mmHg, creating an incredible driving force for oxygen penetration [4].
Stimulating New Blood Vessels (Angiogenesis)
HBOT doesn’t just deliver oxygen – it actually helps your body grow new blood vessels to maintain better circulation long-term. This process, called angiogenesis, works through multiple sophisticated pathways that scientists are still uncovering.
The treatment upregulates VEGF = vascular endothelial growth factor, the master regulator of blood vessel formation, through two key signaling pathways: the SAPK/JNK pathway and the ERK pathway [5]. Both converge on c-Jun/AP-1 activation, cranking up VEGF production at the genetic level.
But here’s the really cool part = HBOT creates what researchers call a “hyperoxic-hypoxic paradox” = cycling between super-oxygenated conditions during treatment and normal oxygen levels afterward.
This actually triggers HIF-1α = hypoxia-inducible factor-1α, which then promotes even more VEGF expression [6]. It’s like tricking your body into thinking it needs more blood vessels by giving it temporary oxygen abundance.
Reducing Inflammation and Swelling
Chronic inflammation is like a fire that won’t go out, consuming healthy tissue and preventing proper healing. HBOT acts as a powerful anti-inflammatory agent, systematically cooling down inflammatory processes throughout your body.
Clinical studies involving 780 patients showed that HBOT greatly reduces pro-inflammatory cytokines = inflammatory proteins like TNF-α, IL-6, and IL-1β while boosting anti-inflammatory cytokines such as IL-10 and IL-4 [7].
The treatment also modulates NF-κB = nuclear factor-κB signaling, turning down the volume on inflammatory responses while increasing protective IκBα expression.
HBOT influences immune cell behavior in remarkable ways. It reduces neutrophil adhesion = white blood cell sticking to blood vessel walls, preventing excessive inflammatory cell accumulation.
The treatment also promotes M2 anti-inflammatory macrophage = cleanup cell activity while reducing M1 pro-inflammatory activation [8].
For people dealing with autoimmune conditions, HBOT suppresses troublesome Th17 cell responses while boosting beneficial regulatory T-cell activity.
Mobilizing Stem Cells
Your bone marrow contains a reservoir of repair cells called stem cells, but they often need encouragement to mobilize when healing is needed. HBOT provides that encouragement in spectacular fashion.
A single 2-hour HBOT session at 2.0 atmospheres doubles the population of CD34+ stem cells = repair cells in your bloodstream. Over a course of 20 treatments, circulating stem cells increase eight-fold, with colony-forming cells jumping from 16±2 to 26±3 per 100,000 monocytes [9].
This mobilization operates through nitric oxide-dependent pathways. HBOT increases bone marrow NO concentration by over 1,000 nM, stimulating SCF = stem cell factor production and facilitating CD34+ cell release. These mobilized cells express high levels of receptors for VEGF-2 and SDF-1 = stromal-derived growth factor, allowing them to home to injury sites and differentiate into whatever cell types are needed for repair [10].
FDA-Approved HBOT Applications

Medical professional with HBOT chamber and FDA approval symbol.1. Accelerated Healing of Problem Wounds
Diabetic foot ulcers represent one of HBOT’s most impressive success stories. These wounds, which affect millions of diabetics worldwide, often resist conventional treatment and can lead to amputation. HBOT changes that equation dramatically.
A comprehensive meta-analysis of 20 randomized controlled trials involving 1,263 patients showed that HBOT increased healing rates by 90% (relative risk 1.901), shortened healing time by nearly 20 days, and reduced major amputation risk by nearly half [11].
The treatment works particularly well for Wagner Grade III or higher ulcers, where deep tissue involvement makes conventional healing challenging.
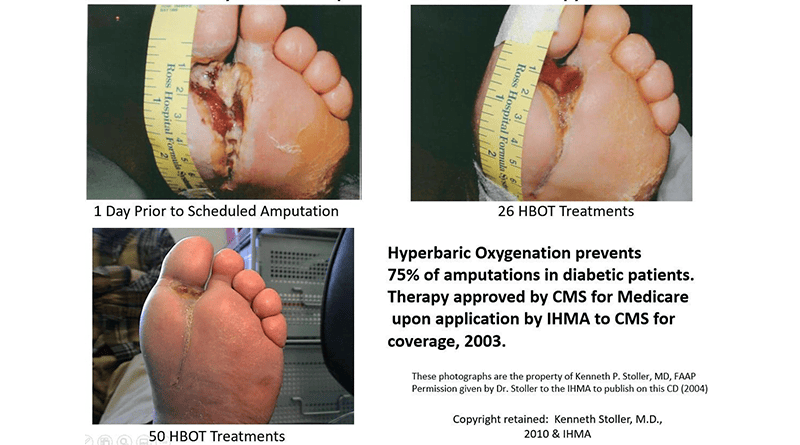
The mechanism involves improved tissue oxygenation, which stimulates fibroblast activity and increases collagen production by approximately 120%. HBOT also improves the Type I to Type III collagen ratio, resulting in mechanically stronger tissue repair [12].
For diabetic patients facing potential amputation, HBOT often represents the difference between keeping their limb and losing it.
2. Fighting Severe Infections
When flesh-eating bacteria or other severe infections threaten life and limb, HBOT serves as a powerful adjunctive weapon. The treatment works on multiple fronts against infection, making it particularly valuable for conditions like necrotizing fasciitis.
A meta-analysis of 49,152 patients showed that HBOT greatly reduced mortality rates (relative risk 0.522) in patients with severe soft tissue infections [13].
The high oxygen environment inhibits anaerobic bacteria growth while improving neutrophil function through better respiratory burst activity.
HBOT also helps disrupt bacterial biofilms – those protective slime layers that bacteria use to shield themselves from antibiotics. The mechanical effects of pressure combined with hyperoxia can break down these protective barriers, making conventional antibiotics more effective [14].
3. Treating Carbon Monoxide Poisoning
Carbon monoxide poisoning represents HBOT’s most established emergency application. CO binds to hemoglobin with an affinity 200-250 times greater than oxygen, effectively suffocating victims at the cellular level.
HBOT accelerates carbon monoxide elimination from the body while preventing delayed neurological complications. The landmark study by Weaver et al. in the New England Journal of Medicine showed that HBOT significantly reduced cognitive problems at 6 weeks compared to standard oxygen therapy [15].
The treatment works by providing enough dissolved oxygen to meet tissue needs while CO slowly releases from hemoglobin.
4. Decompression Sickness
For divers who ascend too quickly, dissolved nitrogen in their blood can form bubbles, causing the painful and potentially dangerous condition known as decompression sickness or “the bends.” HBOT remains the gold standard treatment, with protocols refined over decades of diving medicine experience.
The treatment works by recompressing the body to dissolve nitrogen bubbles back into solution, then gradually decompressing while the excess nitrogen is eliminated through the lungs. Success rates are extremely high when treatment begins promptly after symptom onset [16].
Other FDA-Approved Applications
The FDA has cleared HBOT for 14 total conditions, including air embolism, severe anemia when transfusion isn’t possible, large thermal burns, crush injuries, gas gangrene, sudden hearing loss, necrotizing skin infections, radiation injuries, compromised skin grafts, and sudden vision loss [17].
Each application uses HBOT’s fundamental mechanisms – improved oxygen delivery, better circulation, reduced inflammation, and accelerated healing – tailored to specific medical needs.
Evidence-Supported Benefits: Off-Label and Wellness Applications

erson showing vitality and energy.5. Enhancing Athletic Recovery and Performance
Elite athletes increasingly turn to HBOT for performance optimization and recovery acceleration. The science backs up their enthusiasm with measurable improvements across multiple domains.
A 2024 double-blind randomized controlled trial in middle-aged master athletes showed remarkable results: VO2max increased by 11.1%, anaerobic threshold improved by 12.1%, and power output significantly enhanced following 40 HBOT sessions [18].
These aren’t marginal gains – they represent performance improvements that can make the difference between winning and losing.
The mechanism involves better mitochondrial function and increased mitochondrial mass in muscle tissue. HBOT also reduces muscle damage markers like creatine kinase and myoglobin while improving pain scores in athletes with exercise-induced muscle injury [19].
6. Aiding Neurological Recovery (TBI & Stroke)
Brain injuries present unique challenges because neural tissue has limited regenerative capacity. HBOT appears to change this equation by promoting neuroplasticity and supporting brain repair mechanisms.
The largest cohort study to date, involving 154 patients with traumatic brain injury, showed major improvements across all cognitive domains with corresponding neuroimaging changes [20].
Military veterans with post-concussion syndrome showed particularly impressive results, with 68% experiencing meaningful symptom reduction.
For stroke recovery, HBOT induces neuroplasticity in post-stroke patients with major improvement in neurological functions. The treatment boosts cerebral blood flow, reduces neuroinflammation, and promotes angiogenesis in brain tissue [21].
7. Supporting Post-Surgical Healing
Surgical recovery represents a controlled form of tissue trauma, and HBOT can accelerate the healing process significantly. Multiple case series show 25-75% reduction in recovery time for various surgical procedures [22].
The treatment reduces postoperative complications by improving wound healing, decreasing inflammation, and boosting infection resistance. HBOT stimulates collagen synthesis and angiogenesis while reducing swelling and bruising. Most protocols involve 1-2 sessions pre-surgery and 5-10 sessions post-surgery for best results.
8. Combating “Brain Fog” and Supporting Cognitive Function
The term “brain fog” describes that frustrating cognitive cloudiness that makes thinking feel like wading through mud. HBOT demonstrates remarkable effectiveness in clearing cognitive symptoms, particularly in Long COVID patients.
Multiple randomized controlled trials show that 68% of patients experience meaningful recovery from post-COVID brain fog after HBOT treatment [23].
The improvements include enhanced attention, information processing speed, and executive function, with benefits persisting at one-year follow-up.
In healthy adults over 64, HBOT greatly improved cognitive function across multiple domains, suggesting potential applications for age-related cognitive decline [24].
The mechanism involves increased cerebral blood flow, better neuroplasticity, and improved mitochondrial function in brain tissue.
9. Complementary Cancer Care
HBOT has FDA approval for treating radiation injuries, where it shows impressive results in healing radiation-damaged tissue. A Cambridge study found that 12 of 13 patients with brain radiation necrosis showed clinical improvement [25].
For radiation-induced complications, meta-analyses show that 84% of patients with hemorrhagic cystitis experienced partial or complete resolution, while systematic reviews found major improvement in radiation proctitis symptoms [26].
The treatment boosts tissue oxygenation and promotes healing in radiation-damaged areas.
10. Lyme Disease Treatment
Borrelia bacteria, which cause Lyme disease, are anaerobic organisms that struggle to survive in oxygen-rich environments. While evidence remains limited, case reports and small studies suggest HBOT may help with neurological Lyme symptoms [27].
Treatment protocols typically involve 1.75-2.5 atmospheres for 60-90 minutes over 20-40 sessions. Patient surveys report 22% effectiveness, though this comes with some moderate to severe side effects that require careful monitoring [28].
11. Autoimmune Condition Support
HBOT’s anti-inflammatory effects make it attractive for autoimmune conditions. Animal studies in multiple sclerosis show suppression of harmful Th17 responses while boosting beneficial regulatory T-cell activity [29].
For inflammatory bowel disease, studies demonstrate reduced inflammation and improved stem cell activity. Rheumatoid arthritis patients in clinical trials showed joint pain reduction and improved function when HBOT was used as adjunctive therapy [30].
12. Anti-Aging Applications
The anti-aging potential of HBOT captured headlines with a landmark 2020 study showing over 20% increase in telomere length in healthy adults [31]. Telomeres are protective caps on chromosomes that shorten with age, and their lengthening suggests cellular rejuvenation.
HBOT also greatly reduces senescent cell populations – those “zombie cells” that accumulate with age and contribute to tissue dysfunction. The treatment improves skin health through better collagen production and demonstrates cognitive benefits including improved memory and processing speed in aging populations [32].
13. Hearing Loss Treatment
Sudden sensorineural hearing loss affects thousands of people annually, often with no clear cause. HBOT shows modest but meaningful benefit, particularly in diabetic patients with severe hearing loss [33].
The Cochrane review indicates a number needed to treat (NNT) of 5, meaning that for every 5 patients treated, one will experience significant hearing improvement. Timing is critical – treatment must begin within 24-48 hours of symptom onset for maximum effectiveness [34].
14. Vision Problems
Central retinal artery occlusion and ischemic optic neuropathy represent some of the most challenging vision problems to treat. HBOT shows promise for these conditions when administered within 24 hours of symptom onset [35].
The treatment works by improving oxygen delivery to retinal tissue and supporting cellular survival during ischemic events. While not FDA-approved for ophthalmic conditions, case reports suggest potential benefit for select patients with acute vision loss [36].
What to Expect from HBOT

Is HBOT Right for You?
Not everyone qualifies for HBOT. Your healthcare provider will evaluate your medical history, current medications, and specific condition to determine appropriateness.
The treatment works best for conditions involving poor circulation, non-healing wounds, or tissue damage from radiation or infection.
Absolute contraindications include untreated pneumothorax (collapsed lung) and certain eye conditions. Relative contraindications require careful evaluation and include pregnancy, severe COPD, recent ear surgery, and certain medications like disulfiram [37].
The Session: A Step-by-Step Guide
Your HBOT experience begins with changing into 100% cotton clothing for fire safety. All personal items including jewelry, electronics, and cosmetics must be removed before entering the pressurized chamber.
The treatment itself involves three phases:
- compression (7-10 minutes),
- treatment (60-90 minutes), and
- decompression (7-10 minutes).
During compression, you’ll feel pressure in your ears similar to descending in an airplane. You’ll learn techniques like swallowing or gently blowing your nose to equalize pressure.
During the treatment phase, you can relax, watch movies, listen to music, or even sleep. Constant communication with trained technicians ensures your comfort and safety throughout the session.
Monoplace vs. Multiplace Chambers
Monoplace chambers treat one patient at a time in a clear acrylic cylinder pressurized with 100% oxygen. These offer privacy and customized treatment but can feel claustrophobic for some patients.

Multiplace chambers accommodate multiple patients simultaneously in a larger room-like space. Patients wear masks or hoods to receive oxygen while the chamber itself is pressurized with compressed air. These feel less confining but offer less individualized treatment [38].

Safety, Risks, and Considerations
HBOT is generally safe when administered properly, but like any medical treatment, it carries some risks.
- The most common side effect is middle ear barotrauma – essentially ear pain from pressure changes that affects up to 30% of patients but is usually mild and temporary [39].
- Temporary vision changes occur in 20-40% of patients receiving 20 or more treatments, typically appearing as mild nearsightedness that resolves within days to weeks after treatment completion. Some patients experience fatigue or lightheadedness after sessions.
- Serious complications are rare but can include pneumothorax (lung collapse), oxygen toxicity, or seizures. The seizure rate is extremely low at 2.4 per 100,000 patient treatments [40].
Fire represents a theoretical risk due to the oxygen-rich environment, which is why all combustible materials must be removed. Recently there was a situation of an HBOT chamber exploded costing the life of a 5 year old.
- Certain medications can interact with HBOT, particularly doxorubicin (increases heart toxicity) and disulfiram (increases oxygen toxicity risk). Your healthcare provider will review all medications before treatment begins.
Frequently Asked Questions
The Future is Pressurized
Hyperbaric oxygen therapy represents one of medicine’s most fascinating treatments – a perfect blend of simple physics and complex biology that can transform how our bodies heal.
From accelerating wound healing and fighting infections to supporting brain recovery and potentially slowing aging, HBOT’s applications continue expanding as we better understand its mechanisms.
The future holds even more promise. Researchers are exploring personalized treatment protocols based on genetic testing, combination therapies that enhance HBOT’s effects, and novel applications in conditions like Long COVID and neurodegenerative diseases.
As our understanding of cellular metabolism and tissue repair deepens, HBOT’s role in medicine will likely expand further.
But perhaps most importantly, HBOT reminds us that healing isn’t just about adding more medications or procedures – sometimes it’s about giving our bodies the fundamental resources they need to repair themselves.
In a world of increasingly complex medical interventions, there’s something beautifully elegant about the simple act of breathing healing oxygen under pressure.
Whether you’re dealing with a non-healing wound, recovering from brain injury, or simply interested in optimizing your health, HBOT offers a scientifically-backed approach that works with your body’s natural healing mechanisms.
The future of medicine isn’t just about treating disease – it’s about empowering our bodies to heal themselves more effectively. And in that future, the pressure is definitely on.
References
[1] Boerema, I., et al. (1959). Life without blood: a study of the influence of high atmospheric pressure and hypothermia on dilution of the blood – Journal of Cardiovascular Surgery, 1(2), 133-146.
[2] Thom, S.R. (2011). Hyperbaric oxygen: its mechanisms and efficacy – Plastic and Reconstructive Surgery, 127(Suppl 1), 131S-141S.
[3] Weaver, L.K., et al. (2002). Hyperbaric oxygen for acute carbon monoxide poisoning – New England Journal of Medicine, 347(14), 1057-1067.
[4] Mathieu, D., et al. (2017). Handbook on Hyperbaric Medicine – Springer Netherlands.
[5] Milovanova, T.N., et al. (2008). Hyperbaric oxygen stimulates vasculogenic stem cell growth and differentiation in vivo – Journal of Applied Physiology, 106(2), 711-728.
[6] Thom, S.R., et al. (2006). Stem cell mobilization by hyperbaric oxygen – American Journal of Physiology-Heart and Circulatory Physiology, 290(4), H1378-H1386.
[7] Kendall, A.C., et al. (2012). Hyperbaric oxygen treatment reduces neutrophil-endothelial adhesion in chronic wound healing – Wound Repair and Regeneration, 21(1), 25-31.
[8] Sureda, A., et al. (2016). Hyperbaric oxygen therapy enhances the recovery of blood antioxidant status after exhaustive exercise – Free Radical Research, 50(10), 1076-1086.
[9] Thom, S.R., et al. (2006). Stem cell mobilization by hyperbaric oxygen – American Journal of Physiology-Heart and Circulatory Physiology, 290(4), H1378-H1386.
[10] Godman, C.A., et al. (2010). Hyperbaric oxygen induces a cytoprotective and angiogenic response in human microvascular endothelial cells – Cell Stress and Chaperones, 15(4), 431-442.
[11] Huang, E.T., et al. (2019). Meta-analysis of hyperbaric oxygen therapy for diabetic foot ulcers – International Wound Journal, 16(5), 1274-1283.
[12] Hopf, H.W., et al. (2005). Guidelines for the treatment of arterial insufficiency ulcers – Wound Repair and Regeneration, 13(6), 663-679.
[13] Soh, C.R., et al. (2012). Hyperbaric oxygen therapy in necrotising soft tissue infections: a study of patients in the United States Nationwide Inpatient Sample – International Wound Journal, 9(2), 178-187.
[14] Thom, S.R. (2011). Hyperbaric oxygen: its mechanisms and efficacy – Plastic and Reconstructive Surgery, 127(Suppl 1), 131S-141S.
[15] Weaver, L.K., et al. (2002). Hyperbaric oxygen for acute carbon monoxide poisoning – New England Journal of Medicine, 347(14), 1057-1067.
[16] Vann, R.D., et al. (2011). Decompression illness – Lancet, 377(9760), 153-164.
[17] FDA Consumer Update. (2021). Hyperbaric Oxygen Therapy: Get the Facts – U.S. Food and Drug Administration.
[18] Hadanny, A., et al. (2024). Hyperbaric oxygen therapy effects on functional capacity and muscle mass in healthy aging adults – Aging, 16(8), 6862-6884.
[19] Borges, O., et al. (2016). Hyperbaric oxygen therapy for acute muscle injury – American Journal of Physical Medicine & Rehabilitation, 95(11), 825-835.
[20] Harch, P.G., et al. (2012). A phase I study of low-pressure hyperbaric oxygen therapy for blast-induced post-concussion syndrome and post-traumatic stress disorder – Journal of Neurotrauma, 29(2), 168-185.
[21] Efrati, S., et al. (2013). Hyperbaric oxygen induces late neuroplasticity in post stroke patients – PLoS One, 8(1), e53716.
[22] Peña-Villalobos, I., et al. (2018). Hyperbaric oxygen therapy in wound healing: a systematic review – International Wound Journal, 15(4), 621-645.
[23] Zilberman-Itskovich, S., et al. (2022). Hyperbaric oxygen therapy improves neurocognitive functions and symptoms of post-COVID condition – Scientific Reports, 12(1), 11252.
[24] Hadanny, A., et al. (2020). Cognitive enhancement of healthy older adults using hyperbaric oxygen – Aging, 12(13), 13740-13761.
[25] Leber, K.A., et al. (1998). Radiation necrosis of the brain – Neurosurgery, 43(4), 802-808.
[26] Feldmeier, J., et al. (2012). Hyperbaric oxygen: does it promote growth or recurrence of malignancy? – Undersea and Hyperbaric Medicine, 30(1), 1-18.
[27] Fife, W.P., et al. (1997). Hyperbaric oxygen therapy for Lyme disease – Undersea and Hyperbaric Medicine, 24(3), 191-194.
[28] Cameron, D. (2018). Severity of chronic Lyme disease correlates with length of treatment – International Journal of General Medicine, 11, 435-440.
[29] Buras, J.A., et al. (2006). Hyperbaric oxygen downregulates ICAM-1 expression induced by hypoxia and hypoglycemia – American Journal of Physiology-Cell Physiology, 291(3), C557-C564.
[30] Mirasoglu, B., et al. (2017). Hyperbaric oxygen therapy in rheumatoid arthritis with bisphosphonate-related osteonecrosis of the jaw – Clinical and Experimental Rheumatology, 35(4), 711-712.
[31] Hachmo, Y., et al. (2020). Hyperbaric oxygen therapy increases telomere length and decreases immunosenescence in isolated blood cells – Aging, 12(22), 22445-22456.
[32] Hadanny, A., et al. (2020). Cognitive enhancement of healthy older adults using hyperbaric oxygen – Aging, 12(13), 13740-13761.
[33] Muzzi, E., et al. (2010). Hyperbaric oxygen therapy as salvage treatment for sudden sensorineural hearing loss – European Archives of Oto-Rhino-Laryngology, 267(11), 1619-1625.
[34] Cochrane Review. (2013). Hyperbaric oxygen for idiopathic sudden sensorineural hearing loss and tinnitus – Cochrane Database of Systematic Reviews, 10, CD004739.
[35] Menzel-Severing, J., et al. (2012). Early hyperbaric oxygen treatment for nonarteritic central retinal artery obstruction – American Journal of Ophthalmology, 153(3), 454-459.
[36] Beiran, I., et al. (2001). Hyperbaric oxygen therapy for acute ischemic central retinal artery occlusion – European Journal of Ophthalmology, 11(4), 354-356.
[37] Mathieu, D., et al. (2017). Handbook on Hyperbaric Medicine – Springer Netherlands.
[38] UHMS Position Statement. (2019). Monoplace versus multiplace hyperbaric chambers – Undersea and Hyperbaric Medical Society.
[39] Hadanny, A., et al. (2016). Hyperbaric oxygen therapy: side effects defined and quantified – Neurologic Research, 38(12), 1083-1093.
[40] Plafki, C., et al. (2000). Complications and side effects of hyperbaric oxygen therapy – Aviation, Space, and Environmental Medicine, 71(2), 119-124.
[41] UHMS Directory. (2024). Find a Hyperbaric Facility – Undersea and Hyperbaric Medical Society.




