In modern medicine, hyperbaric oxygen therapy is the process of breathing 100% oxygen in a pressurized chamber exceeding normal atmospheric pressure. This treatment floods body tissues with up to twenty times the normal oxygen concentration, accelerating healing processes and treating conditions ranging from decompression sickness to diabetic wounds.
The journey from primitive air pressure devices to sophisticated medical chambers spans over three centuries.
Understanding this evolution illuminates not just medical history, but humanity’s persistent drive to manipulate the fundamental elements of life – air and pressure – for therapeutic benefit.
What began as crude experiments with bellows and sealed rooms has transformed into a sophisticated medical discipline backed by rigorous science and serving millions worldwide.
History of Hyperbaric Oxygen Therapy
350+ Years of Medical Innovation
The Dawn of Pressurized Air Therapy (Pre-Oxygen Era: 17th-18th Century)
1662: Nathaniel Henshaw’s “Domicilium”
In 1662, British clergyman and physician Nathaniel Henshaw created the first hyperbaric chamber, called the “domicilium,” using a system of organ bellows to change the atmospheric pressure in a sealed chamber.
This contraption wasn’t exactly high-tech – imagine a large wooden box with bellows attached, more barn than hospital.
The Domicilium was a large fifteen-by-fifteen-foot chamber with the capabilities of pressurizing to between two to four atmospheres (ATA). For contrast, modern chambers compress to a max of three atmospheres, typically.
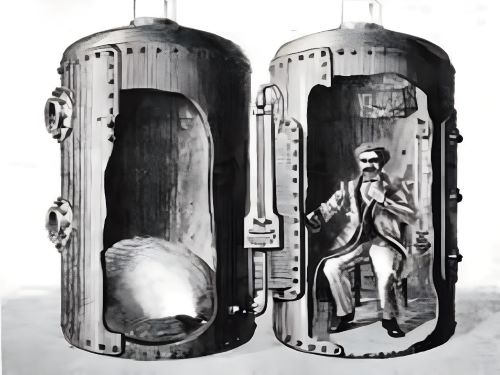
Henshaw operated on a simple theory: “In times of good health, this ‘domicilium’ is proposed as a good resource to aid digestion, promote insensitive breathing, facilitate breathing, and the expulsion of sputum. Consequently, it is extremely useful in preventing most lung infections”.
His logic? Acute conditions would benefit from increased air pressure, while chronic ailments needed decreased pressure.
The impracticality of his proposed method of compressing and decompressing the chamber is readily apparent. So, too, the likely toxic accumulation of carbon dioxide within the unventilated chamber during lengthy laborious periods required to operate it.
(Ed. note: Without proper ventilation or understanding of gas exchange, Henshaw’s patients were essentially suffocating in their own exhaled CO2 – not exactly therapeutic.)
Early Experiments and Observations
In 1666, Robert Boyle’s work “Origin of Forms and Qualities according to the Corpuscular Philosophy” demonstrated that a reduction in ambient pressure could lead to bubble formation in living tissue.
This description of a viper in a vacuum was the first recorded description of decompression sickness. In 1670, Robert Boyle conducted an experiment where he placed a viper (a poisonous snake) in a chamber and rapidly reduced the pressure in that chamber.
Gas bubbles developed in the tissues of the snake—specifically, “a conspicuous bubble moving to and from in the waterish humor of one of its eyes.”
“So the snake had a bubble bouncing around in its eyeball?”
Yes, and this wasn’t some party trick. Boyle had just demonstrated what would later plague deep-sea divers and tunnel workers: decompression sickness.
The intellectual climate of the era was ripe for such discoveries, as natural philosophers began systematically investigating the properties of air and its effects on living organisms.
The Discovery of Oxygen and its Nascent Medical Role (Late 18th – Early 19th Century)
Joseph Priestley Discovers Oxygen (c. 1774)
On August 1, 1774, Joseph Priestley conducted his most famous experiment. Using a 12-inch-wide glass “burning lens,” he focused sunlight on a lump of reddish mercuric oxide in an inverted glass container placed in a pool of mercury. The gas emitted, he found, was “five or six times as good as common air.”
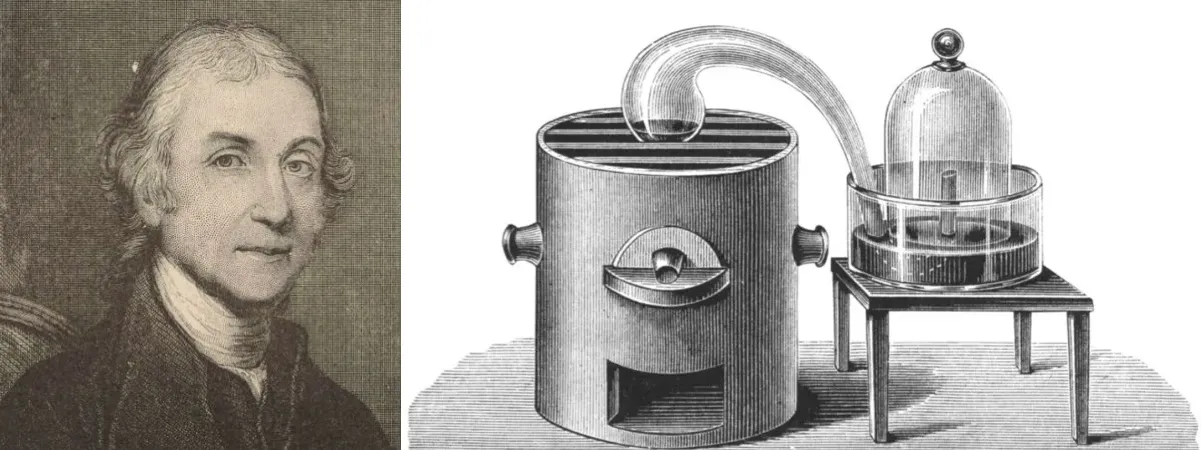
Priestley called his discovery “dephlogisticated air” on the theory that it supported combustion so well because it had no phlogiston in it, and hence could absorb the maximum amount during burning.
The phlogiston theory – now thoroughly debunked – held that combustible materials released a substance called phlogiston when burned. Priestley’s “dephlogisticated air” was actually pure oxygen, though he never abandoned his belief in phlogiston. [1]
Early Cautions and Challenges
Antoine Lavoisier, who named the gas oxygène, meaning acid former, in 1778, would eventually overturn the phlogiston theory entirely. The reason for the delay was the fear of side effects based on the work of Lavoisier and Seguin who had suspected toxic effects of highly concentrated oxygen in 1789.
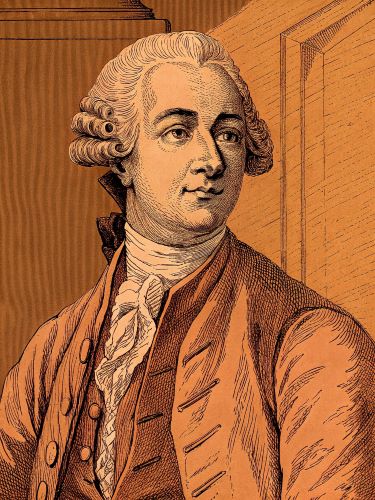
This early recognition of potential oxygen toxicity created a scientific hesitation that would delay the combination of pressurized environments with concentrated oxygen for nearly a century.
The gap between discovering oxygen and using it under pressure represents one of medicine’s great missed opportunities—like having all the ingredients for a cake but being afraid to turn on the oven.
First Documented Medical Use of Oxygen (Non-Hyperbaric)
In 1783 the French physician Caillens treated a young woman with phthisis (tuberculosis) who ‘very much benefited’ from daily inhalations of oxygen. This marked the first therapeutic use of the newly discovered gas, though it would be administered at normal atmospheric pressure.
Thomas Beddoes established the Pneumatic Institution at Dowry Square, Hotwells in 1799. Its first superintendent was Humphry Davy, who investigated the properties of nitrous oxide in its laboratory.
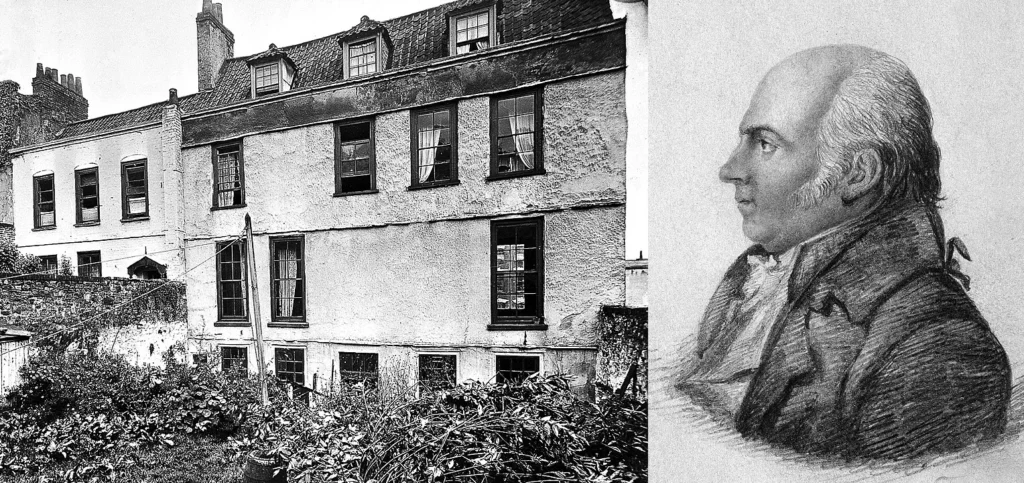
Beddoes believed that various “factitious airs” (artificially produced gases) could treat diseases, particularly tuberculosis.
The “Pneumatic Era”: Compressed Air Baths and Early Chambers (19th Century)
The French Renaissance of Pressure Therapy (1830s onwards)
The 1830s witnessed what could only be described as “chamber fever” sweeping across France.
In 1834, Junod built a hyperbaric chamber to treat pulmonary afflictions using pressures of 2-4 ATA and reported increased circulation to the internal organs, improvements in cerebral blood flow, and production of feelings of well-being.
Between 1837 and 1877 in several cities in Europe (Berlin, Amsterdam, Brussels, London, Vienna, and Milan) the so-called Pneumatic Centers were opened, among which the one founded by Bertin in Montpellier and many rather luxurious pneumatic centers stood out.
These weren’t your typical medical facilities – think Victorian-era health spas with a scientific twist. Wealthy patrons would sit in ornate pressurized rooms, convinced they were receiving cutting-edge treatment for everything from arthritis to “nervous exhaustion.”
In 1837, Pravaz built the largest hyperbaric chamber in Lyon, France, for 12 patients and treated patients with pulmonary conditions such as tuberculosis, laryngitis, tracheitis, and pertussis as well as cholera.
B. Engineering Marvels and Medical Necessity
In 1840, Charles Pasley, charged with the recovery of the sunken warship HMS Royal George, commented that, of those who made frequent dives, “not a man escaped the repeated attacks of rheumatism and cold.”
In 1841, Trigger, a French mining engineer, used a pressure chamber to deliver workers to the bottom of the river to extract coal. In 1845, he reported that some of his miners complained of joint pains and nervous disorders after surfacing.
The industrial revolution had created a new medical emergency: caisson disease. In 1873, Andrew Smith coined the term “caisson disease” to describe 110 cases of decompression sickness during the Brooklyn Bridge construction, which employed 600 compressed air workers but lacked on-site recompression treatment.
In 1879 the French surgeon Fontaine built a mobile operating room on wheels that could be pressurized. He performed over 20 surgeries in the unit using nitric oxide as the anesthetic.
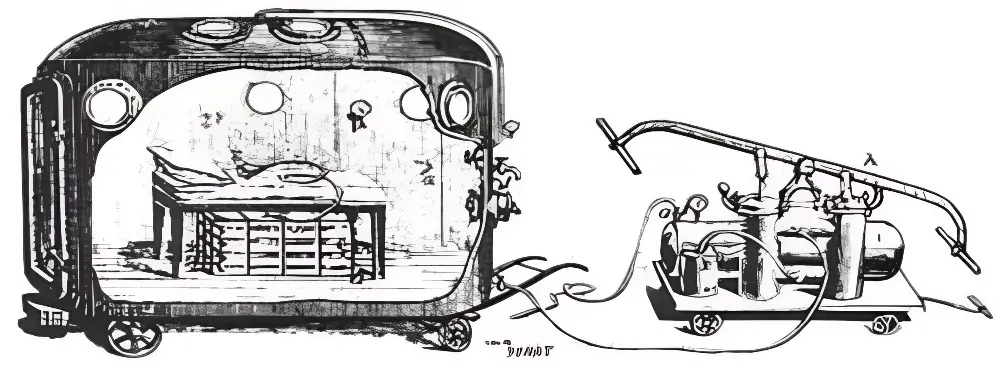
Fontaine noted that he could achieve deep surgical anesthesia because it increased the effective percentage of nitrous oxide in the patient’s body, accompanied by a higher oxygen partial pressure (i.e., compressed air at two atmospheres given an effective level of 42 percent inhaled oxygen).
Paul Bert: The Father of Pressure Physiology (1878)
Central nervous system toxicity was first described by Paul Bert in 1878. He showed that oxygen was toxic to insects, arachnids, myriapods, molluscs, earthworms, fungi, germinating seeds, birds, and other animals.
His masterwork, “La Pression barométrique,” documented a disturbing phenomenon: “We conclude from all these experiments that oxygen does not kill by acting on the heart, the motor nerves, or the muscles, but the reflex acts of the spinal cord… The poisoning is characterized by convulsions”.
The CNS toxic effects of oxygen are hence called ‘Bert effect‘. Bert had discovered that too much of a good thing – even life-giving oxygen – could kill.
His work established the scientific foundation for safe pressure limits that continue to guide hyperbaric medicine today.
Early North American Adoption
The first hyperbaric chamber on the North American continent was built in 1860 in Oshawa, Ontario, Canada, east of Toronto.
The first such chamber in the United States was built by Corning a year later in New York to treat ‘nervous and related disorders’.
ℹ️ Did You Know?
Physicist Edward Teller (father of the hydrogen bomb) was so impressed by HBOT after his stroke treatment that he purchased his own hyperbaric chamber for home use.
The Marriage of Pressure and Oxygen: Birth of Modern HBOT (Early 20th Century)
Pioneering Work in Decompression Sickness
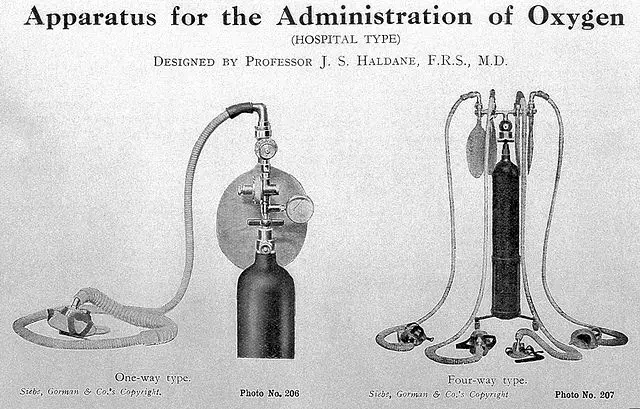
In 1908 Haldane developed the Admiralty decompression tables I and II. John Scott Haldane’s methodical approach to preventing decompression sickness revolutionized diving safety. His concept of “staged decompression”—ascending slowly with planned stops—remains the foundation of safe diving practice.
Dr. Orville J. Cunningham used high partial pressure of oxygen to treat hypoxic states, and observes that patients with heart problems and circulatory disorders, who felt bad living in the mountains, they improved at sea level.
During the 1918 Spanish flu pandemic, this professor put a young doctor who was dying of suffocation in a hyperbaric chamber that he used for animal experiments, and saved his life by compressing him to 2 atmospheres.
In 1928, Cunningham built the largest hyperbaric chamber in the world in Cleveland, Ohio. This “Hyperbaric Hotel” was a five-story high steel sphere at 64 feet in diameter. (Ed. note: Picture a giant steel ball with windows—part hospital, part Jules Verne fantasy.) At that time, it was the only hyperbaric chamber operating in the world.
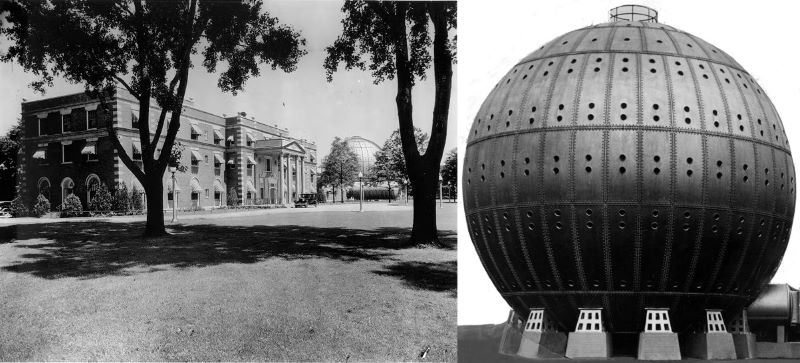
This “ball of steel” hospital, located in Cleveland (Ohio), had inside a smoking room on the top floor, dining rooms and individual rooms and pressurized up to 3 ATA.
Wait, a smoking room? In a pressurized oxygen environment? The mind boggles at the safety standards—or lack thereof—of the era.
Behnke and Shaw: First Use of Hyperbaric Oxygen for Decompression Sickness (1937)
In 1937, Behnke and Shaw successfully used hyperbaric oxygen to treat decompression sickness. This was the first effective use of HBOT for a specific medical condition.
They replaced oxygen in place of compressed air, and their work resulted in the use of the first nitrogen-oxygen mixtures and hyperbaric treatment being tailored to the severity of the injury.
This represented a fundamental shift in thinking. No longer was it just about pressure – it was about delivering concentrated oxygen under pressure. The therapeutic possibilities suddenly expanded exponentially.
Expanding Applications Before and During WWII
In 1938, Brazilians Ozorio de Almeida and Costa pioneered the use of HBOT in treating leprosy.
In 1942, End & Long used HBOT for Carbon Monoxide Poisoning. The war years accelerated research as military physicians sought treatments for wounded soldiers and submarine crews.
The Mid-Century Boom: HBOT Gains Clinical Acceptance (1950s-1970s)
Dr. Ite Boerema: The “Father of Modern Hyperbaric Medicine” (1950s-1960s)
In the 1950s, Ite Boerema, a cardiac surgeon from the Netherlands, conceived the idea of “flooding” the body’s tissues with extra oxygen.
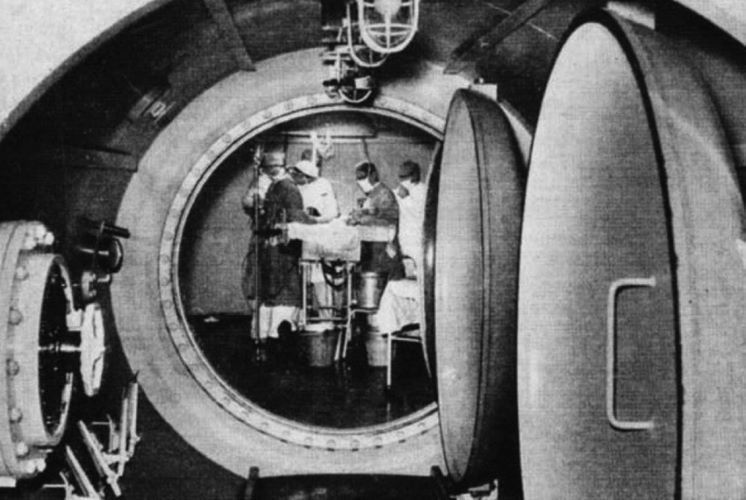
His most famous experiment reads like science fiction: In 1960, Dr. Boerema published a study on “life without blood.” It involved exsanguinating pigs and removing their erythrocytes before exposing them to 3 ATM of HBO. These pigs were noted to have sufficient oxygen in the plasma to sustain life.
The implications were staggering. The researchers found that pigs inhaling oxygen at a pressure of 3 atmospheres could survive for periods of 15 minutes, with only 0.4% hemoglobin. If plasma alone could carry enough oxygen to sustain life, what other medical impossibilities might hyperbaric oxygen make possible?
Boerema achieved wide recognition in Europe and the United States and was known as a hard-worker with great amounts of motivation and determination with endless passion for medicine and science.
He approached surgery as “engineering in medicine,” treating the human body as a complex machine that could be optimized through precise application of physical principles.
Churchill-Davidson: Radiosensitivity of Tumors (1955)
In 1955, Churchill-Davidson used hyperbaric oxygen therapy to enhance radiation therapy for cancer patients. The logic was elegant: tumors often have hypoxic cores that resist radiation. Flood them with oxygen, and suddenly they become vulnerable to treatment.
ℹ️ Did You Know?
According to legend, Alexander the Great was lowered into the Bosphorus Straits in a glass vessel, making him possibly the first person to experience increased atmospheric pressure underwater (circa 332 BC).
Growing List of Indications
In 1961, a colleague of Boerema, W. H. Brummelkamp, published a paper on inhibition of anaerobic infections by HBOT. The treatment of gas gangrene—a rapidly spreading, often fatal infection—became one of HBOT’s most dramatic success stories.
The 1960s saw an explosion of applications: crush injuries, acute traumatic ischemias, necrotizing soft tissue infections. Each success built upon the last, creating momentum for wider acceptance.
Formalization and Professionalization
In 1967 the Undersea Medical Society (UMS) was founded by six U.S. Navy Diving and Submarine medical officers as an organization dedicated to diving and undersea medicine. The UMS was later renamed Undersea and Hyperbaric Medical Society (UHMS) in 1986.
The American College of Hyperbaric Medicine was founded by Dr. Neubauer in 1983. These organizations brought scientific rigor to a field that had too often relied on anecdote and enthusiasm.
Consolidation and Expansion (Late 20th Century – Early 21st Century)
Mainstream Integration
By the 1980s, HBOT had shed its reputation as fringe medicine. The Centers for Medicare & Medicaid Services initiated reimbursement for HBOT for the treatment of diabetic foot ulcer (DFU) in 2002.
(Insurance coverage = mainstream acceptance in American medicine).
Technological Advancements
The clunky steel spheres of Cunningham’s era gave way to sleek, computer-controlled chambers. Modern, low-pressure monoplace chambers represent significant advancements from earlier designs, improving the therapy’s accessibility and affordability.

Patients could now watch movies during treatment, communicate with technicians, and—crucially—not feel like they were trapped in a submarine.
Expanding Research Horizons
The 21st century has seen HBOT research branch into previously unimaginable territories.
Traumatic brain injury, stroke, inflammatory conditions, even potential cancer treatment adjuncts – the list grows yearly. Current uses of HBOT span from treating decompression sickness and aiding wound healing to exploring potential improvements in neurological conditions.
Modern HBOT: Current Status and Approved Indications
The FDA currently recognizes HBOT for treating: [2]
- Decompression sickness (“the bends”)
- Air or gas embolism
- Carbon monoxide poisoning
- Crush injuries and compartment syndromes
- Diabetic wounds
- Enhanced healing of problem wounds
- Necrotizing soft tissue infections
- Osteomyelitis (bone infections)
- Radiation tissue damage
- Skin grafts and flaps at risk
- Severe anemia
- Thermal burns
- Idiopathic sudden sensorineural hearing loss
- Central retinal artery occlusion
The FDA advises you get the treatment at a hospital or facility that has been inspected and is accredited by the Undersea and Hyperbaric Medical Society.
Challenges, Skepticism, and Re-evaluation in HBOT’s History
HBOT’s history includes spectacular failures alongside its successes. The American Medical Association (AMA) and the Cleveland Medical College, having no scientific justification for its treatments, forced its closure in 1930. Cunningham’s sanitarium, for all its grandeur, was demolished for scrap metal during World War II.
The field has constantly battled between enthusiasts making extravagant claims and skeptics dismissing legitimate applications.
The FDA is aware there are some hyperbaric oxygen treatment centers promoting hyperbaric oxygen chambers for uses that have not been cleared or approved by the FDA, such as treatment of cancer, Lyme disease, autism, or Alzheimer’s disease.
“Is HBOT a miracle cure for everything?”
No, and that’s precisely the point. The challenge has always been separating scientifically validated uses from wishful thinking. This tension between promise and proof continues to shape the field.
The Future of Hyperbaric Oxygen Therapy
Where does HBOT go from here? Current research suggests we’ve barely scratched the surface. Personalized protocols based on individual physiology, combination therapies that amplify HBOT’s effects, portable chambers for home use – the possibilities expand as our understanding deepens.
The fundamental insight remains unchanged from Henshaw’s time: oxygen and pressure, properly applied, can achieve remarkable healing.
What’s changed is our ability to apply these forces precisely, safely, and with scientific understanding of the mechanisms involved.
Conclusion
From Henshaw’s bellows-powered domicilium to computer-controlled chambers delivering precise oxygen doses, HBOT’s journey reflects medicine’s broader evolution. What began as intuition – that pressure and air could heal—has become sophisticated science.
The story isn’t just about technology. It’s about persistent human curiosity, the willingness to challenge conventional thinking, and the sometimes centuries-long gap between discovery and application. Priestley discovered oxygen in 1774, but it took until 1937 for Behnke and Shaw to combine it with pressure for treating decompression sickness. Such delays remind us that medical progress rarely follows a straight line.
Today, as researchers explore HBOT’s potential for conditions from autism to Alzheimer’s, we’re writing new chapters in this centuries-old story. The spirit of innovation that drove Henshaw, Priestley, Bert, and Boerema continues.
We’ve learned to harness one of nature’s most fundamental forces – the healing power of oxygen under pressure. The journey continues, one breath at a time.
References / Further Reading
- Breath of life: the evolution of oxygen therapy – PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC1079621/ - History of HBO – DDRC Healthcare
https://www.ddrc.org/hyperbarics/history-of-hbo/ - Hyperbaric oxygen therapy: the history – DVM360
https://www.dvm360.com/view/hyperbaric-oxygen-therapy-history - History of the hyperbaric chamber – Biobarica
https://www.biobarica.com/en/news/history-of-the-hyperbaric-chamber-jWo2k097pH3Xe3hPXksM/ - History of Oxygen Therapy – Wessex MS Therapy Centre
https://www.wessexms.co.uk/history-oxygen-therapy - Rev Henshaw – Hyperbarics & The Domicilium
https://oxygens.co.uk/rev-henshaw-hyperbarics-the-domicilium/ - The History of Hyperbaric Oxygen Therapy: From Medical Innovation to Premium Health Solution – Aviv Clinics
https://aviv-clinics.com/blog/hbot/the-history-of-hyperbaric-oxygen-therapy-from-medical-innovation-to-premium-health-solution/ - What is the history of Hyperbaric Oxygen Therapy? – Oxygen Oasis
https://www.o2oasis.com/what-is-the-history-of-hyperbaric-oxygen-therapy/ - Brief Amazing History of Hyperbaric Medicine – Watts HBOT
https://www.wattshbot.com/post/brief-amazing-history-of-hyperbaric-medicine - Historical Aspects of Hyperbaric Physiology and Medicine – IntechOpen
https://www.intechopen.com/chapters/66258 - Diving into the Past: A Comprehensive History of Hyperbaric Oxygen Therapy – Plus by APN
https://plusapn.com/hbot/history-of-hyperbaric-oxygen-therapy/ - Paul Bert • LITFL • Medical Eponym Library
https://litfl.com/paul-bert/ - Oxygen toxicity – Wikipedia
https://en.wikipedia.org/wiki/Oxygen_toxicity - Robert Boyle – Wikipedia
https://en.wikipedia.org/wiki/Robert_Boyle - Joseph Priestley – Wikipedia
https://en.wikipedia.org/wiki/Joseph_Priestley - Antoine Lavoisier – Wikipedia
https://en.wikipedia.org/wiki/Antoine_Lavoisier - Undersea and Hyperbaric Medical Society – Wikipedia
https://en.wikipedia.org/wiki/Undersea_and_Hyperbaric_Medical_Society - Paul Bert – Wikipedia
https://en.wikipedia.org/wiki/Paul_Bert




