- Research shows higher number of hyperbaric oxygen therapy sessions significantly decreases death risk, especially for critical infections.
- Nighttime sessions and administration of catecholamines identified as important risk factors requiring special attention.
- First 72 hours of treatment prove crucial for patient survival, with proper protocols and staff training essential for safety.
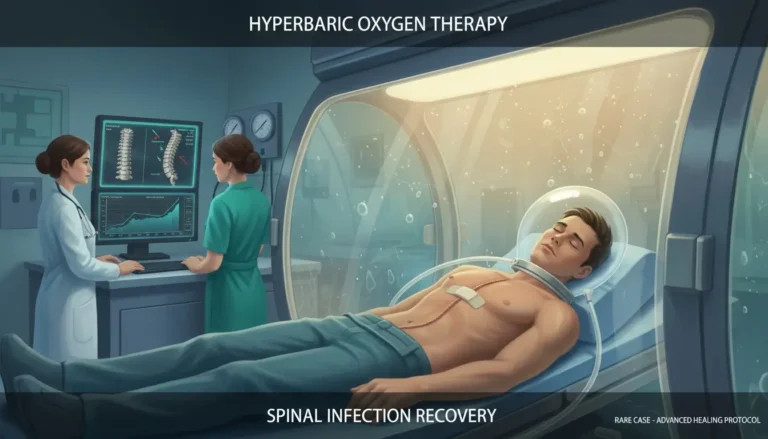
A comprehensive ten-year study conducted at the University Centre for Maritime and Tropical Medicine in Gdynia, Poland has revealed important findings about the safety and efficacy of hyperbaric oxygen therapy (HBOT) for critically ill patients. The research, published in Scientific Reports, analyzed data from 176 intensive care patients who received HBOT while requiring mechanical ventilation between 2013 and 2023.
The study led by Aneta Miszewska and colleagues identified several risk factors during transport and HBOT sessions but ultimately demonstrated that when properly administered, HBOT can significantly improve survival rates for patients with severe conditions, particularly necrotizing soft tissue infections (NSTI) and gas gangrene.
Understanding Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy involves patients breathing pure oxygen in a pressurized chamber for approximately 90 minutes at pressures greater than 1.5 atmospheres absolute. This treatment dramatically increases oxygen levels in the bloodstream, which can help fight bacteria, reduce inflammation, and promote healing in patients with critical conditions.
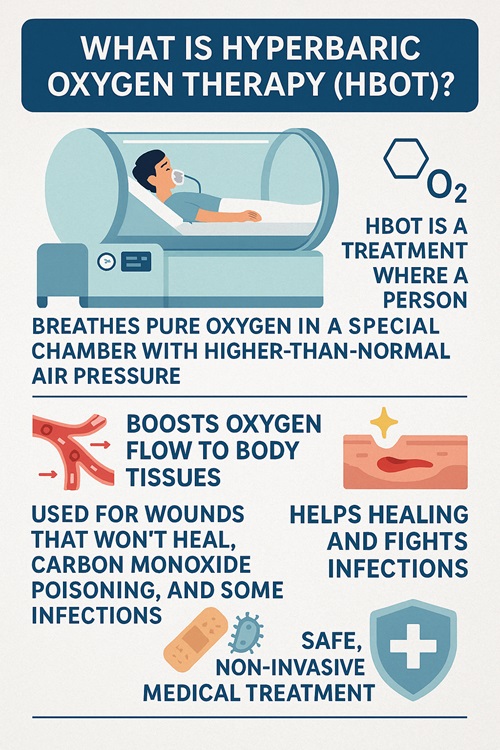
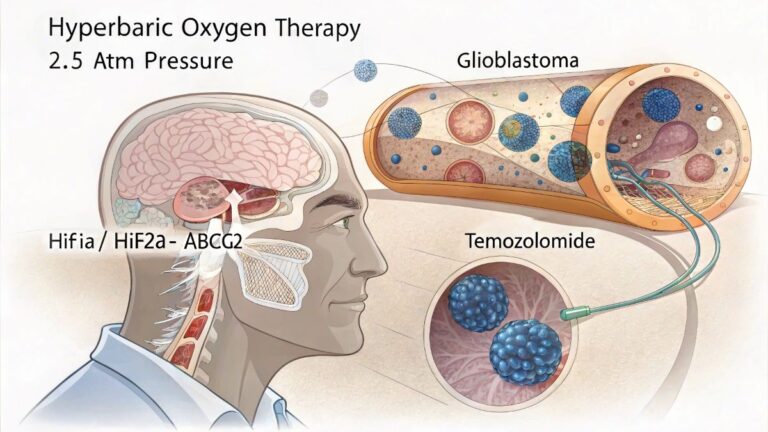
The therapy is particularly valuable for life-threatening conditions such as carbon monoxide poisoning, necrotizing soft tissue infections, crush injuries, air and gas embolism, decompression illness, acute thermal burns, and intracranial abscesses.
However, providing this therapy to critically ill patients presents unique challenges. Dr. Jacek Kot, co-author of the study, explains that the hyperbaric environment itself creates specific physiological changes and potential risks that must be carefully managed, especially for mechanically ventilated patients.
Risk Factors and Safety Protocols
The study identified several key risk factors that require careful attention:
- Mechanical ventilation: All patients in the study required breathing assistance through endotracheal tubes, which necessitated special modifications to prevent tracheal trauma during pressure changes.
- Medication infusions: The research found that continuous infusion of catecholamines (medications that support blood pressure and heart function) significantly increased mortality risk, with a relative risk of 3.56.
- Nighttime sessions: Over half (56.55%) of all HBOT sessions occurred during night shifts, when staff performance is potentially compromised by fatigue. The researchers noted that cognitive function is poorest between 4:00 am and 6:00 am, precisely when many sessions were scheduled.
- Transportation challenges: Moving critically ill patients between the ICU and hyperbaric chamber presents inherent risks, though the facility’s design with the chamber in close proximity to the ICU helped minimize these dangers.
- Special equipment needs: Patients with pleural cavity drainage (6.25%) or requiring hemodiafiltration (21.02%) needed additional precautions, as these treatments can be affected by pressure changes.
Despite these challenges, the study reported only two deaths (1.14%) occurring during actual HBOT sessions over the ten-year period, both involving patients in extremely critical condition with septic shock upon admission.
Survival Benefits
Perhaps the most significant finding was that increasing the number of HBOT sessions substantially improved survival rates, with each additional session reducing the risk of death by 29% (RR = 0.71, p < 0.001).
“The number of HBOT sessions demonstrated a statistically significant association with a reduced risk of death,” the researchers reported in their findings.
The overall mortality rate in the study was 15.90%, which compares favorably to other research reporting higher mortality rates for similar patient populations without HBOT intervention. Previous studies have shown mortality rates as high as 89.6% for NSTI patients in intensive care settings.
The researchers identified that the first 72 hours of treatment were particularly crucial for patient survival. During this period, patients received appropriate antibiotic therapy, underwent radical wound debridement when needed, and had increased frequency of HBOT sessions.
Facility and Staff Considerations
The study highlighted several factors that contributed to the relatively low mortality rate:
- The facility’s unique design integrated the ICU and hyperbaric chamber in the same building, minimizing transport time and risks.
- The same medical team provided care to patients both in the ICU and during HBOT sessions, ensuring continuity of care.
- Staff were highly trained in both intensive care and hyperbaric medicine.
- Ward beds were adapted for use in the hyperbaric chamber, eliminating the need for transfers.
Dr. Miszewska emphasized that maintaining this level of care requires substantial investment in staff education and training. Research has consistently shown a clear relationship between healthcare provider education levels and patient outcomes, with higher levels of education associated with improved safety and better clinical results.
Implications for Future Practice
The researchers provided three key conclusions based on their findings:
- HBOT performed on ICU patients following applicable standards, with qualified staff and adapted equipment, ensures clinical safety during transport and treatment.
- Patients with severe infections (NSTI and gas gangrene) require special attention due to their higher risk of adverse events and mortality.
- The first 72 hours of hospitalization for critically ill patients receiving HBOT are crucial for survival.
While the study demonstrated significant benefits, it also acknowledged limitations, including the possibility that some critically ill patients may not have been referred for HBOT due to transportation challenges, potentially skewing mortality data. Additionally, the study only examined in-hospital mortality without tracking long-term outcomes after discharge.
What does this mean for the future of critical care? The integration of hyperbaric medicine into intensive care protocols could save more lives, especially for patients with necrotizing infections and other severe conditions. However, this requires specialized facilities, extensive staff training, and careful risk management.
As hospitals consider incorporating HBOT into their treatment options for critically ill patients, this research provides valuable guidance on safety protocols, risk factors, and potential benefits. The evidence suggests that when properly implemented, hyperbaric oxygen therapy can be a powerful tool in the intensive care arsenal, offering hope for patients with some of the most challenging medical conditions.
Research Reference
- Study Title: Safety of intensive care hyperbaric oxygen therapy sessions at a tertiary academic hospital
- Authors: Aneta Miszewska, Jacek Kot, Ewa Lenkiewicz
- Journal: Scientific Reports (2025) 15:12131
- DOI: https://doi.org/10.1038/s41598-025-97226-6
- Study Period: 2013-2023
- Sample Size: 176 ICU patients requiring mechanical ventilation and HBOT
- Key Finding: Each additional HBOT session reduced mortality risk by 29% (RR = 0.71, p < 0.001)