- Hubert Allen completed 60 hyperbaric oxygen treatments at the ECU Health Wound Healing Center.
- The therapy addressed complications from a radiation injury that left him wheelchair-bound.
- Allen now walks and drives independently.
- Dr. Jamie Udwadia directed the medical care.
- The treatment enhances oxygen delivery to promote tissue healing.
Hubert Allen, a resident of Roanoke Rapids, North Carolina, regained his ability to walk and drive after completing 60 sessions of hyperbaric oxygen therapy (HBOT) at the ECU Health Wound Healing Center.
The treatment targeted complications from a radiation injury, which caused chronic wounds, frequent hospital stays, and disorientation.
As the first patient to reach this milestone at the center, Allen’s recovery highlights the role of advanced wound care in restoring independence. The facility, part of ECU Health North Hospital, provides outpatient services including HBOT for non-healing wounds.
Patient’s Recovery Path
Allen started treatment on May 1 at the center located at 244 Smith Church Road. Before therapy, the radiation injury limited his mobility and daily activities.
The medical team, including Dr. Jamie Udwadia, nurse practitioner Ashley Duke, and manager Jennifer Millius, oversaw his care.
Allen praised the staff, saying “The ECU Health Wound Healing Center team was extremely compassionate and supportive during my treatments.”
As reported in the Roanoke Rapids Daily Herald, his progress allowed him to leave his wheelchair behind.
Therapy Process and Benefits
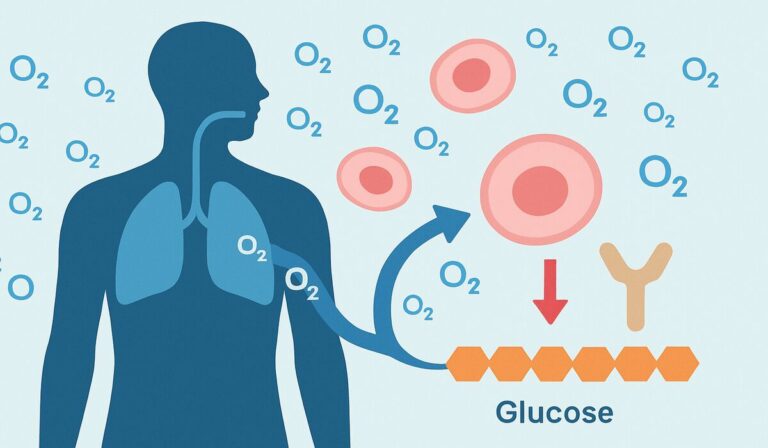
HBOT delivers 100% oxygen in a pressurized chamber, increasing blood oxygen levels to aid healing in damaged tissues.
For radiation injuries, it counters reduced blood flow and promotes new vessel growth, known as angiogenesis. Protocols often involve 20 to 60 sessions, each lasting about 100 minutes, at pressures of 2 to 3 atmospheres absolute (ATA).
According to the National Center for Biotechnology Information (NCBI) StatPearls, this approach suits delayed radiation effects like osteoradionecrosis and cystitis, with evidence from studies by Robert Marx showing improved outcomes when combined with surgery.
Dr. Udwadia explained the method, noting:
“Hyperbaric oxygen therapy restores at the cellular level. Hubert’s radiation injury was slowing his healing, but today, his recovery is a testament to the power of modern medicine and personal resilience.”
The center uses monoplace chambers compatible with standard medical monitoring equipment.

Radiation injuries
Radiation injuries often occur months or years after cancer treatments, involving damage to blood vessels through obliterative endarteritis and the release of fibrogenic cytokines such as transforming growth factor-beta (TGF-beta).
This leads to hypoxic, hypovascular, and hypocellular tissues, complicating healing. HBOT addresses these by delivering pure oxygen at elevated pressures, typically 2 to 3 ATA, which enhances oxygen saturation in plasma and supports cellular repair.
Sessions occur in monoplace or multiplace chambers, with patients monitored for compatibility with devices like ventilators if needed.
Allen’s experience aligns with established protocols. For mandibular osteoradionecrosis, researcher Robert Marx recommended 20 preoperative HBOT sessions followed by 10 postoperative ones, combined with antibiotics to prevent complications. In broader soft tissue cases, up to 60 sessions may apply, as in Allen’s treatment. Evidence from a 1985 randomized trial by Marx and colleagues showed HBOT outperforming penicillin alone in preventing bone necrosis. The Undersea and Hyperbaric Medical Society guidelines support HBOT for late effects of radiation therapy (LERT), with about one-third of U.S. HBOT cases addressing such injuries.
Potential Risks of HBOT
Potential risks of HBOT include barotrauma to ears or sinuses from pressure changes, temporary myopia after prolonged use, and rare oxygen toxicity seizures. Contraindications cover untreated pneumothorax and certain chemotherapy agents. Facilities like ECU Health adhere to safety standards, ensuring patient screening and supervision by certified staff.
To outline HBOT applications for radiation injuries, consider the following table based on clinical evidence:
| Condition | Key Features | HBOT Protocol | Supporting Evidence |
|---|---|---|---|
| Osteoradionecrosis (jaw) | Bone death from vascular damage, common in head/neck cancer patients. | 20-30 sessions at 2.4 ATA, pre- and post-surgery. | Marx RE (1985) randomized trial; improved healing rates vs. antibiotics alone. |
| Radiation Cystitis | Bladder inflammation and bleeding post-pelvic radiation. | 30-40 sessions, 2-2.5 ATA. | Reduces hematuria; Medicare-approved indication. |
| Soft Tissue Necrosis | Tissue death in irradiated areas like chest or abdomen. | Up to 60 sessions, combined with wound care. | Enhances graft survival; Feldmeier JJ (2012) review. |
| Radiation Proctitis | Rectal bleeding and fibrosis from pelvic treatments. | 20-40 sessions at 2 ATA. | Improves symptoms via angiogenesis; literature supports adjunct use. |
| Laryngeal Radionecrosis | Cartilage damage in throat post-radiation. | Variable sessions, focused on pre-surgical preparation. | Prevents complications in reconstructive procedures. |
Allen’s story, as covered in recent reports from September 2025, underscores community-based access to HBOT, reducing travel burdens for rural patients.
ECU Health’s network, including similar centers at Roanoke-Chowan Hospital, extends these services across the region.
While individual outcomes vary based on injury severity and radiation exposure, cases like this provide evidence for HBOT’s role in multidisciplinary wound care.